Did you know that ovarian cancer is the fifth most common cause of cancer-related death among women, with only about 30% of patients surviving beyond five years when diagnosed at advanced stages? Unfortunately, about 95% of high-grade cases are detected late, drastically reducing survival chances.
Preventive healthcare offers a promising alternative to this reactive approach. Instead of waiting for symptoms to appear, preventive healthcare solutions focus on identifying disease biomarkers early—before clinical manifestations occur.
What is Preventive healthcare in today’s digital age? It’s a revolutionary approach where artificial intelligence analyzes biological signals that traditional screening methods might miss. The difference between preventive and reactive healthcare becomes clear when you consider that early detection of ovarian cancer increases survival rates to 84% for localized disease, compared to just 32% for distant disease.
Thanks to AI algorithms, preventive healthcare strategies now include analyzing complex, high-dimensional datasets and integrating multimodal information from omics, electronic health records, and wearable devices.
Modern preventive healthcare screening has achieved remarkable accuracy, with some AI models demonstrating 92% accuracy and 90% sensitivity in early cancer detection. Additionally, by leveraging longitudinal data from electronic health records rather than single-point measurements, these systems can avoid common temporal biases that plague traditional diagnostic approaches. The vast amount of biological data available today serves as the foundation for effective biomarker analysis, bridging the gap between complex datasets and actionable health insights.
AI and Neural Networks in Preventive Healthcare Solutions
The shift toward preventive care is fundamentally changing healthcare delivery. This approach emphasizes health promotion over disease treatment, creating a paradigm where intervention begins long before symptoms appear [1]. This transformation is especially significant as healthcare systems worldwide embrace predictive, preventive, personalized, and participatory (P4) medicine principles.
What is preventive healthcare in the AI era?
Preventive healthcare in the AI era represents a systematic approach to identifying disease risk factors before clinical manifestations occur. Unlike traditional preventive measures, AI-powered solutions analyze vast amounts of data from multiple sources, including genomics, bioengineering, wearable devices, and electronic health records[1]. Through continuous monitoring, these systems detect subtle deviations from baseline health metrics, enabling immediate intervention at the earliest signs of potential problems [2].
Consider chronic conditions like diabetes or hypertension—conditions that exist on a continuous spectrum between health and disease. While conventional methods might classify individuals as “prediabetic” or “prehypertensive” based on periodic checkups, AI-driven preventive healthcare provides real-time biomarker analysis to detect these conditions at much earlier stages [1].
Furthermore, one study demonstrated that machine learning models could predict prediabetes and type 2 diabetes with 99.5% sensitivity and 99.07% accuracy [1], illustrating the remarkable precision of these technologies.
Neural networks vs traditional models in early detection
Traditional predictive approaches rely primarily on regression-based statistical algorithms, which struggle to handle complex datasets such as repeated biomarker measurements [3]. Neural networks, however, excel at finding hidden relationships between predictive markers and health outcomes without explicit programming [3].
For biomarker detection specifically, different neural network architectures serve distinct functions:
-
Feedforward neural networks process static biomarker features
-
Recurrent Neural Networks (RNNs) and Long Short-Term Memory (LSTMs) networks analyze sequential biomarker data
-
Transformer models integrate multi-modal information
The superiority of neural networks becomes apparent through performance metrics. For instance, in heart disease prediction, gradient boosting machines achieved F1 scores of 84.3% and accuracy of 82.2% while minimizing bias across demographic groups [2]. Similarly, in skin cancer classification, AI algorithms demonstrated 87.0% sensitivity and 77.1% specificity, outperforming clinicians’ 79.8% sensitivity and 73.6% specificity [4].
Perhaps most importantly, neural networks excel at temporal modeling—analyzing patterns over time—which helps avoid the point-in-time bias common in traditional diagnostic approaches that rely on single measurements [5]. Through continuous analysis of longitudinal data, these models capture the progression of biomarkers, offering a more complete clinical picture [5].
Preventive healthcare strategies powered by AI
The integration of AI into preventive healthcare has spawned several effective strategies. First among these is continuous monitoring through wearable devices, which track various physiological parameters such as heart rate, glucose levels, and sleep patterns [6]. Holisticare.io‘s app exemplifies this approach by providing real-time deviation alerts from established biomarker baselines, empowering both patients and healthcare providers with actionable insights.
Clinical data analysis through machine learning also enables personalized lifestyle interventions. For example, an AI-enabled precision health and lifestyle coaching program for adults with type 2 diabetes showed that 71% of participants achieved an A1C of 6.5% or lower—significantly better than control groups using traditional coaching [6]. Moreover, a Johns Hopkins study found that AI-powered diabetes-prevention programs achieved similar health outcomes to traditional programs, but with higher engagement: 93% of participants began the AI program versus 83% in the human-led version [6].
The distinction between prognostic vs predictive capabilities is crucial for clinical decision support. While prognostic models forecast general disease risks, predictive models identify which specific interventions will benefit individual patients. Both approaches serve to empower longevity coaches with informational suggestions, though these always require professional clinical review before implementation [2].
Healthcare systems that deploy AI-based preventive analytics consistently report 10-20% reductions in readmission rates, with some cases showing up to 50% reduction where proactive workflows are implemented [2]. Additionally, medication adherence and preventive care directed by machine learning has been shown to reduce five-year hospitalization risk by over 38.3% [2].
Data Sources for Biomarker Discovery and Prediction
The foundation of any preventive healthcare solution lies in the quality and diversity of data sources it utilizes. As technologies advance and costs decline, researchers now access unprecedented volumes of biological information for biomarker discovery and analysis.
Multi-omics data: genomics, proteomics, metabolomics
Multi-omics approaches integrate multiple layers of biological data to provide a comprehensive view of disease processes. Essentially, these technologies enable researchers to move beyond single-omic approaches that capture only partial biological pictures [7].
What is a biomarker in the context of multi-omics? It represents measurable indicators across different biological levels that collectively reveal disease mechanisms. The integration of these layers creates powerful opportunities:
-
Genomics + Transcriptomics: Revealing whether genetic mutations affect gene expression
-
Proteomics + Metabolomics: Identifying how altered proteins cause metabolic changes
-
Microbiomics + Host genomics: Understanding microbe-host interactions [8]
This multi-dimensional approach significantly enhances biomarker analysis, capturing disease processes at multiple levels simultaneously, revealing causal mechanisms, and supporting better patient stratification [8].
Electronic health records and wearable sensor data
Wearable sensors generate real-time physiological and behavioral data that traditional clinical measurements cannot capture. These devices track numerous health parameters, including:
-
Heart rate, blood pressure, and oxygenation
-
Body temperature and metabolic markers
-
Physical motion, gait, and posture
Subsequently, this data transmits wirelessly to connected devices where AI models transform sensor signals into clinically relevant parameters [10]. Indeed, the integration of AI with wearable sensors allows continuous health monitoring in real-time, creating opportunities for personalized preventive healthcare strategies [1].
Digital biomarkers derived from these sensors can detect subtle physiological changes, identify early warning signs, and enable tailored interventions [10]. Notably, studies show remarkable compliance with wearable protocols—one study achieved 99% valid wear days in clinical settings and 97% in home environments [1].

Longitudinal vs cross-sectional data: why it matters
The distinction between longitudinal and cross-sectional data collection profoundly impacts biomarker discovery. Cross-sectional studies capture data at a single point in time—essentially a snapshot—whereas longitudinal studies follow the same subjects over extended periods [11].
Longitudinal data collection offers decisive advantages for preventive healthcare screening. Primarily, it establishes sequences of events, detects developments or changes at both group and individual levels, and suggests cause-and-effect relationships [11]. Consequently, this approach helps avoid the point-in-time bias common in traditional diagnostic methods that rely on single measurements.
Consider cholesterol monitoring: a cross-sectional study might compare levels among different populations of walkers and non-walkers at one moment, while a longitudinal approach tracks changes in a single group over years, providing deeper insights into causal relationships [11].
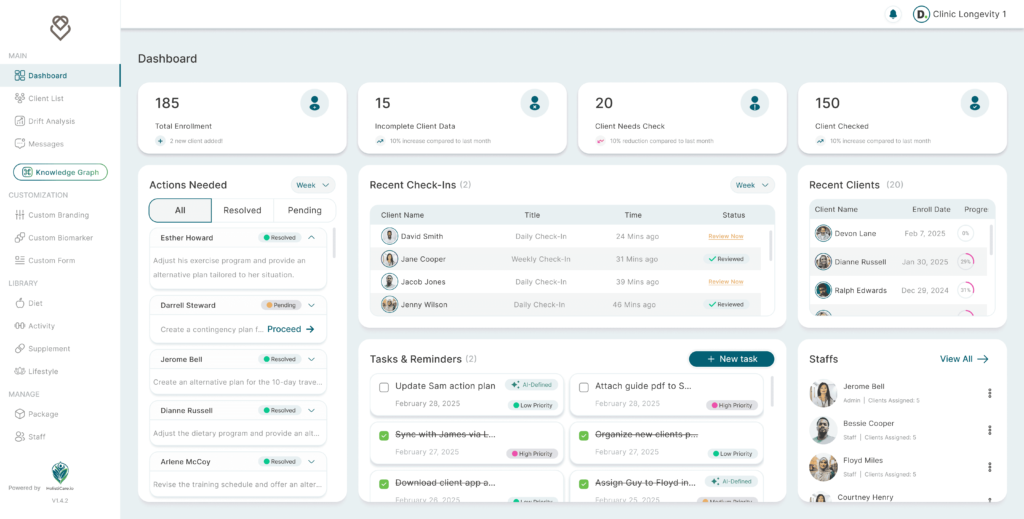
Holisticare's app: real-time deviation alerts from biomarker baselines
HolistiCare exemplifies advanced preventive healthcare solutions through its comprehensive data integration platform. The system ingests multi-vendor data from lab information systems, genetic vendors, and wearable APIs, standardizing it into a canonical model [12]. This includes unit standardization, reference range harmonization, and preservation of raw artifacts for future auditing [12].
Rather than presenting clinicians with isolated abnormal results, HolistiCare identifies meaningful patterns and ranks them by probable impact [12]. The platform’s clinical decision support system combines explicit clinical heuristics with probabilistic models that consider age, sex, medications, and comorbidities [12].
Through its mobile app, HolistiCare delivers real-time deviation alerts when biomarkers stray from established baselines. This hybrid approach combines patient-reported outcomes with device data to create multi-source signals that improve specificity and reduce false positives [5]. For instance, a heart failure monitoring program pairs daily weight checks with symptom reporting to detect fluid retention early [5].
This prognostic vs predictive approach empowers longevity coaches with informational suggestions while ensuring all automated inferences display clinician-readable rationales, including which values drove the inference, relevant thresholds, and linked references [12].
Neural Network Models for Early Biomarker Detection
Neural networks provide the computational backbone for modern preventive healthcare solutions, utilizing specialized architectures to process different types of biomarker data. Their ability to identify subtle patterns that traditional statistical models might miss makes them particularly valuable in early disease detection.
Feedforward neural networks for static features
Feedforward neural networks excel at processing static biomarker features through multiple processing layers. These networks, particularly Multi-Layer Perceptrons (MLPs), analyze predictor variables through activation functions to output results. The architecture typically consists of input, hidden, and output layers that collectively enable classification of samples based on transcriptome data or other static biomarkers. When utilized for colon cancer prediction with processed RNA-seq data, canonical machine learning algorithms achieved 97.33% accuracy [3].
RNNs and LSTMs for sequential biomarker data
For time-series biomarker analysis, Recurrent Neural Networks (RNNs) and Long Short-Term Memory (LSTM) networks demonstrate superior performance. Unlike traditional models, these architectures maintain internal memory that captures temporal relationships in sequential data. In Alzheimer’s disease prediction using neuropsychological measures and MRI biomarkers, LSTM-based approaches achieved 88.24% accuracy, surpassing conventional algorithms [13]. Furthermore, LSTMs predict biomarker values at future time points (6, 12, 18, 24, and 36 months), enabling early intervention before clinical symptoms appear [13].
Transformer models for multi-modal integration
Transformer architectures represent a significant advancement in handling multimodal biomarker data. Through self-attention mechanisms and encoder-decoder structures, these models process sequential data in parallel, resulting in faster training and improved performance [14]. A transformer-based model combining chest radiographs with clinical parameters achieved an impressive AUC of 0.84, compared to 0.83 for radiographs alone and 0.67 for clinical parameters alone [15]. This integration capability makes transformers particularly valuable for comprehensive biomarker analysis across genomics, imaging, and clinical data.
Temporal modeling to avoid point-in-time bias
Traditional biomarker analysis often suffers from temporal bias—an overemphasis on features collected near case events rather than distributed evenly across time [16]. Neural networks overcome this through sophisticated temporal modeling. Time-dependent LSTM (TdLSTM) networks specifically address irregular time intervals in longitudinal data, dynamically adjusting memory content based on elapsed time between measurements [17]. This approach produces significantly lower relative errors (0.453 on baseline data, 0.377 on follow-up data) compared to conventional models [17].
For clinical decision support systems, this temporal modeling capability enables both prognostic and predictive functions. Holisticare.io leverages these advanced neural network architectures to deliver real-time deviation alerts when biomarkers stray from established baselines, empowering longevity coaches with actionable insights while maintaining the requirement for professional clinical review.
Real-World Applications and Clinical Use Cases
Neural networks have moved beyond theoretical applications to transform real-world clinical practice. Their ability to detect subtle patterns in biomarker data enables early intervention across multiple disease states.
Early cancer detection using CA-125 and HE4
Biomarker Analysis for ovarian cancer now combines CA-125 and HE4 serum levels to achieve remarkable detection accuracy. When used together, these biomarkers detect ovarian cancer with an area under the curve (AUC) of 0.77 [18]. Even more impressive, HE4 in combination with BMI and parity predicts endometrial cancer in pre-menopausal women with an AUC of 0.91, offering 84.5% sensitivity and 80.9% specificity [6]. Undeniably, HE4 outperforms CA-125 as a diagnostic biomarker (AUC 0.76 vs. 0.71) [6], highlighting how preventive healthcare screening has evolved beyond single-marker analysis.
Predicting treatment response in chronic diseases
Deep neural networks now enhance Clinical Decision Support by detecting features beyond traditional clinical assessment. For instance, in systemic sclerosis trials, AI-derived fibrosis scores capture skin features that clinicians cannot detect through simple pinch tests [4]. Regarding chronic disease management, Char-RNN models process missing values more effectively than conventional approaches, achieving superior accuracy in predicting conditions like hypertension and stroke [19].
Continuous monitoring with wearables and EHR integration
Preventive healthcare solutions now seamlessly integrate wearable data with electronic health records. Currently, 60% of US adults track health metrics like weight and diet, while 33% monitor specific indicators such as blood pressure [20]. Eventually, these integrated systems enable earlier intervention—as demonstrated by Kaiser Permanente’s virtual cardiac rehab program, which achieved an 87% completion rate with less than 2% readmissions [21].
Empowering longevity coaches with AI insights
Longevity coaching platforms leverage AI to deliver personalized recommendations based on continuous biomarker tracking. Throughout ongoing monitoring, users experience 37% lower rates of metabolic syndrome and biological age markers that are 19% younger than their actual age [22]. Beyond simple analytics, these preventive healthcare strategies incorporate both prognostic risk assessment and predictive intervention suggestions, though all require professional clinical review before implementation [23].
Barriers to Clinical Adoption and Future Outlook
Despite remarkable advances in neural networks for preventive healthcare, several challenges hinder widespread clinical adoption. Addressing these barriers remains crucial for translating promising research into practical healthcare solutions.
Data harmonization and population diversity
The healthcare industry generates approximately 30% of the world’s data volume, with a compound annual growth rate expected to reach 36% by 2025 [24]. Nevertheless, this wealth of information brings harmonization challenges. Biomarker measurements frequently differ across studies due to variations in specimen collection methods, processing procedures, and laboratory platforms [2]. Furthermore, algorithmic bias compounds existing inequities when training data lacks diversity, potentially causing misleading predictions and large-scale discrimination [24].
Regulatory and infrastructure challenges
Regulatory complexity presents another significant hurdle. In Europe, AI-powered healthcare technologies must navigate multiple overlapping frameworks, including the Medical Devices Regulation, In Vitro Diagnostic Medical Devices Regulation, and the AI Act [25]. Accordingly, the U.S. takes a more sectoral approach, with the FDA considering medical AI primarily as medical devices requiring approval before marketing [25]. Given these complexities, healthtech companies may benefit from integrating regulatory readiness into core business strategy rather than treating compliance as an afterthought [26].
Explainable AI for clinical trust and transparency
Clinical Decision Support systems utilizing AI face adoption barriers related to transparency. Clinicians express concern about the lack of explainability regarding how algorithms arrive at recommendations—a contradiction to evidence-based medicine’s foundation [24]. In contrast to common assumptions, studies show explanations sometimes have no significant effect on clinician trust [27]. This mismatch between explanation format and established mental models can increase cognitive load, ultimately impairing performance [27].
The future of preventive healthcare: digital twins and virtual labs
Looking forward, digital twins offer personalized preventive healthcare by creating virtual models that continuously update with real-time biomarker data. Once validated, these applications will expand from controlled areas like early diabetes management to complex conditions such as cancer [28]. Alongside this advancement, temporal modeling will help avoid point-in-time bias through platforms like Holisticare.io, which provides real-time deviation alerts from biomarker baselines. Throughout this evolution, what is a biomarker will expand beyond static measurements to include dynamic, multi-dimensional indicators across biological systems.
Conclusion
Neural networks have fundamentally transformed preventive healthcare through their remarkable ability to detect subtle biomarker changes long before clinical symptoms appear. These advanced systems now analyze multi-dimensional data across genomics, proteomics, and metabolomics, providing unprecedented insights into disease progression patterns. Accordingly, healthcare providers can intervene at optimal times rather than reacting to fully developed conditions.
Temporal modeling stands out as a critical advancement that helps you avoid the point-in-time pitfalls common in traditional diagnostic approaches. Unlike conventional methods that capture single snapshots of health metrics, neural networks analyze longitudinal data to establish meaningful trajectories. Therefore, biomarker analysis becomes significantly more accurate when examined across time rather than in isolation.
What is a biomarker in this new paradigm? Essentially, it has evolved from a static measurement to a dynamic, context-rich indicator that gains meaning through its relationship with other biological signals. This comprehensive understanding enables both prognostic risk assessment and predictive intervention recommendations tailored to individual patients.
Clinical data analysis through AI systems like Holisticare.io demonstrates how real-time deviation alerts from established baselines can empower both patients and healthcare professionals. Though these systems generate informational suggestions for longevity coaches, all automated inferences still require professional clinical review before implementation—maintaining the crucial balance between technological innovation and clinical expertise.
The distinction between prognostic vs predictive capabilities remains crucial for effective clinical decision support. While prognostic models forecast general disease trajectories, predictive approaches identify which specific interventions will benefit particular individuals. Together, these complementary functions create a robust framework for preventive healthcare strategies.
Despite regulatory challenges and data harmonization issues, the future of preventive healthcare appears promising. Digital twins and virtual labs will undoubtedly expand personalized medicine capabilities, while improved explainability will enhance clinician trust and adoption. As these technologies mature, you might soon experience healthcare systems that not only treat diseases but also actively prevent them through continuous monitoring and early intervention.
The preventive healthcare revolution ultimately represents a fundamental shift from reactive to proactive medicine. By detecting biomarkers early through neural networks, analyzing longitudinal data to avoid temporal bias, and providing actionable insights through platforms like Holisticare.io, modern healthcare can finally fulfill its promise of keeping people healthy rather than merely treating them when sick.
Key Takeaways
Neural networks are revolutionizing preventive healthcare by detecting disease biomarkers before symptoms appear, dramatically improving patient outcomes and survival rates.
• Early detection saves lives: AI-powered biomarker analysis increases ovarian cancer survival rates from 32% to 84% when caught early, demonstrating the life-saving potential of preventive screening.
• Temporal modeling beats snapshots: Neural networks analyze longitudinal data patterns over time, avoiding the point-in-time bias that limits traditional diagnostic methods relying on single measurements.
• Multi-modal integration enhances accuracy: Combining genomics, proteomics, wearable data, and electronic health records through transformer models achieves superior detection rates compared to single-source approaches.
• Real-time monitoring enables proactive care: Platforms like Holisticare.io provide continuous biomarker tracking with instant deviation alerts, empowering both patients and healthcare providers with actionable insights.
• AI outperforms traditional methods: Neural networks demonstrate 92% accuracy in early cancer detection and achieve 99.5% sensitivity in diabetes prediction, significantly surpassing conventional diagnostic approaches.
The future of healthcare lies in this shift from reactive treatment to proactive prevention, where continuous monitoring and AI-driven insights keep people healthy rather than simply treating them when sick.
FAQs
Q1. How do neural networks improve early disease detection? Neural networks analyze complex biomarker data to identify subtle patterns that traditional methods might miss. They can detect disease indicators before clinical symptoms appear, significantly improving early diagnosis and treatment outcomes.
Q2. What is the advantage of using longitudinal data in preventive healthcare? Longitudinal data allows for temporal modeling, which helps avoid point-in-time bias common in traditional diagnostic approaches. By analyzing health metrics over time, neural networks can establish meaningful trajectories and provide more accurate biomarker analysis.
Q3. How does AI integration with wearable devices enhance preventive healthcare? AI-powered wearable devices enable continuous health monitoring in real-time. They can track various physiological parameters and detect subtle changes, allowing for personalized preventive healthcare strategies and early intervention.
Q4. What role do multi-omics data play in biomarker discovery? Multi-omics approaches integrate multiple layers of biological data (e.g., genomics, proteomics, metabolomics) to provide a comprehensive view of disease processes. This integration enhances biomarker analysis by capturing disease mechanisms at multiple levels simultaneously.
Q5. How do AI-powered preventive healthcare solutions impact clinical outcomes? AI-based preventive analytics have shown significant improvements in clinical outcomes. For instance, they’ve been reported to reduce hospital readmission rates by 10-20%, and in some cases, reduce five-year hospitalization risk by over 38% through improved medication adherence and preventive care.
References
[1] – https://www.nature.com/articles/s41746-024-01151-3
[2] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11062831/
[3] – https://www.mdpi.com/1424-8220/23/6/3080
[4] – https://medicine.yale.edu/news-article/systemic-sclerosis-ai-deep-neural-networks/
[5] – https://holisticare.io/features/check-ins/
[6] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9689358/
[7] – https://www.sciencedirect.com/science/article/pii/S2215017X25000657
[8] – https://www.revvity.com/blog/biomarker-discovery-era-multi-omics
[9] – https://www.obviohealth.com/resources/sensors-wearables-and-digital-biomarkers-the-current-and-future-state-of-digital-instruments-in-clinical-research
[10] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11147994/
[11] – https://www.iwh.on.ca/what-researchers-mean-by/cross-sectional-vs-longitudinal-studies
[12] – https://holisticare.io/features/clinical-data-analysis-software/
[13] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8874990/
[14] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11316220/
[15] – https://pubs.rsna.org/doi/abs/10.1148/radiol.230806
[16] – https://www.nature.com/articles/s41467-021-21390-2
[17] – https://www.medrxiv.org/content/10.1101/2024.09.25.24314409v2.full-text
[18] – https://aacrjournals.org/cancerdiscovery/article/15/1/105/750840/Early-Detection-of-Ovarian-Cancer-Using-Cell-Free
[19] – https://www.mdpi.com/2076-3417/9/10/2170
[20] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6746089/
[21] – https://tateeda.com/blog/integrate-wearable-into-ehrs-with-ai-intelligence
[22] – https://decodeage.com/blogs/news-1/ultimate-guide-to-ai-longevity-coaching?srsltid=AfmBOopSdPshbQxHZF_jEOlM-2V3kT7Cd8OCG6hzzVHrCx1ujCV4R0Mo
[23] – https://www.profi.io/blog/artificial-intelligence-in-longevity-medicine
[24] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11393514/
[25] – https://law.stanford.edu/2024/04/06/eu-and-us-regulatory-challenges-facing-ai-health-care-innovator-firms/
[26] – https://www.fenwick.com/insights/publications/the-new-regulatory-reality-for-ai-in-healthcare-how-certain-states-are-reshaping-compliance
[27] – https://www.nature.com/articles/s41746-025-02023-0
[28] – https://med.stanford.edu/medicine/news/current-news/standard-news/medical-digital-twins.html
Disclaimer
The information in this article is provided by HolistiCare for general informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. HolistiCare does not warrant or guarantee the accuracy, completeness, or usefulness of any information contained in this article. Reliance on any information provided here is solely at your own risk.
This content does not create a doctor-patient relationship. Clinical decisions should be made by qualified healthcare professionals using clinical judgment and all available patient information. If you have a medical concern, contact your healthcare provider promptly.
HolistiCare may reference biomarker roles, study examples, products, or tools. Mention of specific tests, biomarkers, therapies, or vendors is for illustrative purposes only and does not imply endorsement. HolistiCare is not responsible for the content of third party sites linked from this article, and inclusion of links does not represent an endorsement of those sites.
Use of HolistiCare software, services, or outputs should be in accordance with applicable laws, regulations, and clinical standards. Where required by law or regulation, clinical use of biomarker information should rely on validated laboratory results and regulatory approvals. HolistiCare disclaims all liability for any loss or damage that may arise from reliance on the information contained in this article.
If you are a patient, please consult your healthcare provider for advice tailored to your clinical situation. If you are a clinician considering HolistiCare for clinical use, contact our team for product specifications, regulatory status, and clinical validation documentation.