Did you know that nearly 60% of functional medicine practitioners report feeling overwhelmed by the demands of running their business? Functional medicine scalability has become a critical challenge as providers struggle to balance patient care with administrative tasks.
The problem is clear: modern longevity testing generates over 800+ biomarkers per patient , creating a massive data overload that traditional analysis methods simply cannot handle. Meanwhile, the demand for functional medicine continues to rise as more people seek personalized and holistic healthcare solutions . This documentation burden is at the heart of practitioner burnout solutions being sought across the industry. However, there’s promising news on the clinical intelligence ROI front.
By implementing healthcare operational efficiency systems like HolistiCare, which integrates health data from various sources and applies AI-driven analysis , practitioners can automate patient protocols and save approximately 15 hours per week. This represents a 56% reduction in preparation time, transforming your role from data entry clerk to Chief Health Strategist.
In this article, you’ll discover exactly how to reclaim those 15 hours weekly while scaling your practice without the burnout that comes from wearing too many hats and maintaining inefficient systems . Let’s explore the practical steps to make functional medicine scalability work for you, not against you.
The Real Cost of Data Overload in Functional Medicine
The data deluge in functional medicine isn’t just overwhelming—it’s financially and professionally unsustainable. Functional medicine practitioners face an unprecedented challenge as patient records expand beyond manageable limits, creating ripple effects that impact both practice viability and practitioner wellbeing.
Why 800+ biomarkers per patient is unsustainable
Functional lab tests can include hundreds of biomarkers, examining everything from hormone metabolites and nutrient levels to inflammation markers and gut microbiome diversity [1]. This wealth of information, though valuable, creates significant interpretation challenges. Many of these tests include biomarkers not yet supported by strong clinical evidence, placing results in a confusing “gray zone”—neither definitively harmful nor proven helpful [1]. Furthermore, the advent of high-throughput technologies has complicated the extraction of meaningful molecular signatures from these complex datasets [2]. Without proper guidance, patients and practitioners alike end up with information overload, resulting in anxiety and no clear action plan [1]. As one physician notes, “I don’t recommend using programs that run hundreds of tests without understanding your history, symptoms, or goals,” precisely because such an approach leads to analytical paralysis rather than clinical clarity [1].
How documentation time leads to practitioner burnout
Documentation burden directly correlates with clinician burnout syndrome—a finding consistently supported by research [3]. Approximately 38% of nurses report experiencing at least one burnout symptom [3]. The statistics become more alarming when examining documentation requirements: nurses document between 600-800 data points per 12-hour shift—equivalent to recording one data point every 1.11 minutes [3]. This relentless documentation pace creates emotional exhaustion, which research shows significantly correlates with the volume and time required to complete paperwork [3]. Poor electronic health record (EHR) usability compounds these issues, contributing to both increased documentation burden and heightened burnout risk [3]. Consequently, national turnover rates for healthcare professionals continue to climb, with each replacement costing upwards of $40,000 per position [3].
The hidden ROI of solving data complexity
The financial implications of data overload extend far beyond practitioner burnout. Most functional medicine practices unknowingly leave more than $297,000 in Chronic Care Management revenue unclaimed due to operational inefficiencies [4]. Additionally, each manual patient interaction costs substantially more than automated alternatives—traditional call centers cost $5.63+ per conversation compared to under $1.00 for AI-powered solutions [4]. The real damage, nonetheless, comes from indirect costs: lost revenue opportunities, missed quality bonuses, and the financial impact of clinical team burnout [4]. Indeed, when systems integrate effectively, key information loads automatically at the point of care, reducing documentation time by up to 27% per patient encounter [5]. This improvement in interoperability directly impacts financial returns by cutting unnecessary costs, reducing claim denials, and eliminating workflow delays that slow down both clinical and operational processes [5].
The 15-Hour Weekly ROI: What It Looks Like in Practice
Time is the most precious asset for functional medicine practitioners. Clinicians spend approximately 28 hours per week on administrative duties [6], with medical staff dedicating even more (34 hours weekly) to paperwork and bureaucratic tasks [6]. In fact, administrative costs now account for more than 40% of total expenses hospitals incur when delivering care [6].
From data entry to Chief Health Strategist
The traditional approach to functional medicine involves hours of manual data analysis and documentation. According to research, 49% of physician time goes to EHR and administrative activities, leaving only 27% for actual patient care [6]. This administrative overload dramatically reduces patient interaction time.
With modern clinical intelligence platforms, you can transition from data processor to strategic health advisor. AI automation in documentation saves up to two hours per provider daily [6]. Moreover, these systems handle routine communications, freeing your staff from repetitive tasks.
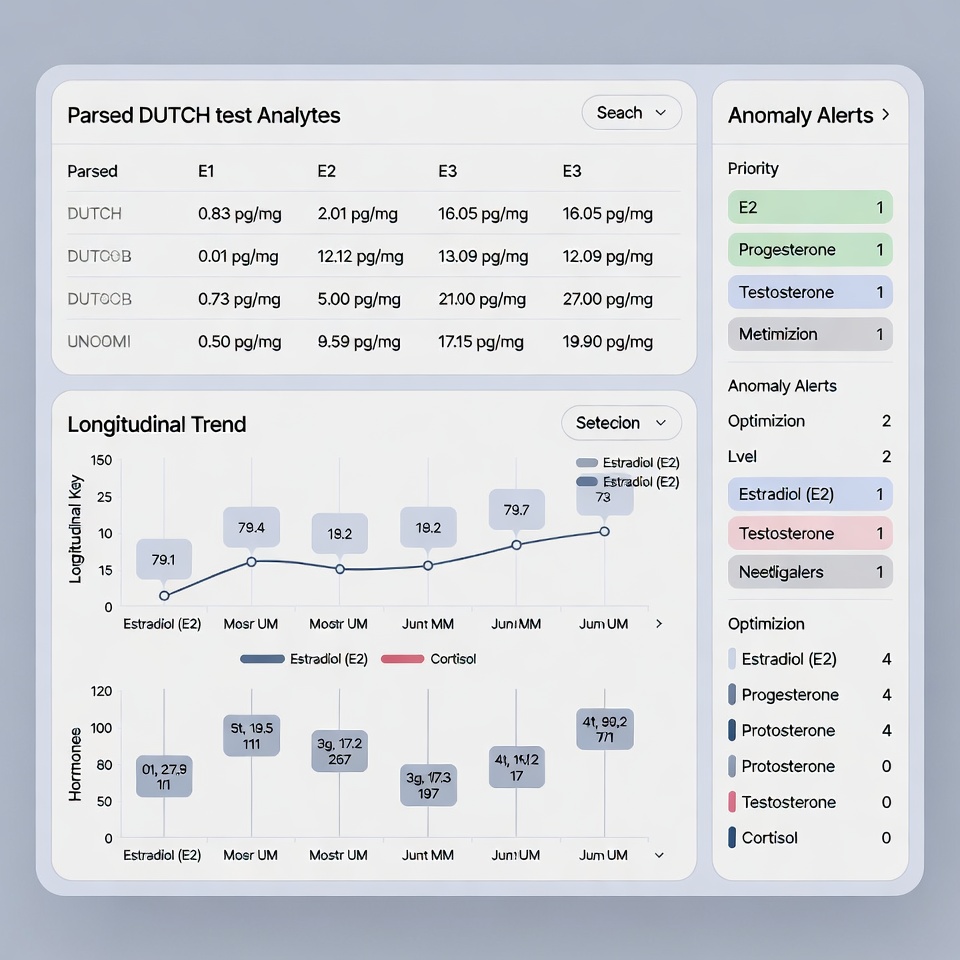
How HolistiCare automates patient protocols
HolistiCare integrates health data from laboratories, wearables, and questionnaires, then applies AI-driven analysis to generate personalized holistic health plans [1]. Specifically, the platform analyzes 800+ biomarkers from blood, genetics, and lifestyle data, creating protocols that sound as if you wrote them personally [1].
The system combines biomarkers, genetics, lifestyle, and behavior into clinician-reviewable holistic plans spanning diet, exercise, sleep, and mental health domains [1]. Furthermore, it uses clinician-directed customization to set preferences, escalation rules, and monitoring cadences [1].
Case example: Weekly time savings breakdown
The real-world impact of automation on functional medicine scalability is substantial:
HolistiCare reduces the time needed to produce first drafts of clinical reports by 56%, cutting average preparation time from 180 hours to just 80 hours [6]. This acceleration allows you to deliver personalized recommendations without lengthy delays.
AI-powered drafting tools maintain quality standards during this accelerated process, actually decreasing error rates by 50% across categories including data accuracy, terminology, and citations [6]. In essence, you gain approximately 15 hours weekly while improving accuracy and maintaining personalized care—the perfect solution for practitioner burnout challenges.
4 Clinical Intelligence Workflows That Save Time
Four essential workflows now make functional medicine scalability possible without sacrificing quality care. These intelligent systems address the root causes of practitioner burnout while enhancing patient outcomes.
1. Unified patient data workspace
A unified patient workspace integrates clinical data, AI interpretation, and operational workflows so teams can efficiently assess and engage patients [1]. This comprehensive approach creates a single authoritative record with complete data history from labs, genetics, and wearables [1]. Instead of having “more” information, unified data ensures the right information appears at the right time [7]. When information flows seamlessly across systems, providers receive full context for better decision-making [7]. This integration effectively closes gaps when data is fragmented, helping practitioners spot what’s missing [8].
2. AI-generated holistic care plans
AI powered by longevity-focused knowledge graphs generates tailored holistic plans for diet, exercise, mental health, and lifestyle ready for clinician review [1]. These systems analyze a patient’s comprehensive health profile to recommend treatments combining conventional approaches with complementary therapies [2]. By examining patient data and clinical outcomes, AI uncovers trends not easily detected by clinicians [9]. This approach allows practitioners to rapidly generate care plans reflecting each patient’s unique biology and preferences [10].
3. SMART task scheduling and delivery
Based on client preferences, AI schedules personalized action plans and delivers tasks directly to mobile apps for real-world adherence [1]. Features include SMART task creation, multichannel delivery, and preference-aware scheduling [1]. Intelligent scheduling tools using data-driven algorithms can automate administrative tasks and improve patient interactions [11]. These systems typically boost physician utilization rates between 87%-98% [11]. Time blocking—reserving specific hours for defined activities—aligns with natural energy patterns for optimal workflow [12].
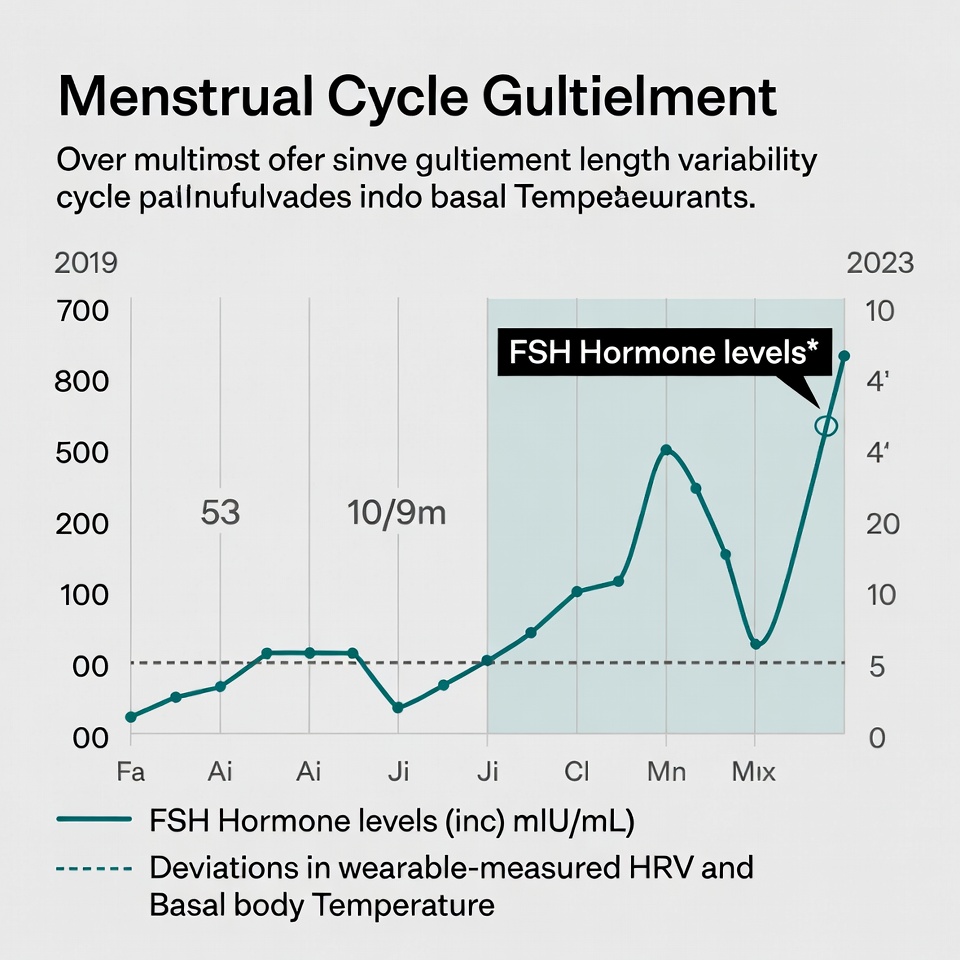
4. Real-time patient monitoring and alerts
With mobile apps, practitioners stay connected to clients while AI monitors vitals, tracks deviations, and answers questions in real-time [1]. Remote patient monitoring gathers continuous data on physiological conditions, allowing earlier identification of health deterioration [13]. This consistent monitoring enables prompt care interventions and decreases unnecessary clinic visits [13]. Practitioners can view valuable health information patients might not report during appointments [13]. Additionally, wearable technology helps detect problems early by providing continuous health metrics between office visits [3].
Building a Scalable Practice Without Burnout
Building a successful functional medicine practice requires structural changes, not just working harder. Chronic conditions affect approximately 60% of adults, with 42% having multiple conditions [14]. Creating a sustainable practice means addressing both clinical excellence and business viability simultaneously.
Redesigning your role as a practitioner
Traditional primary care physicians see 25-30 patients daily to maintain practice viability, whereas functional medicine requires 60-90 minute initial consultations [15]. Your role must shift from doing everything yourself to strategic oversight. Many practitioners launch with passion but without a clear business model, leading to burnout from excessive one-on-one sessions [16]. Consider alternative models like monthly memberships or bundled programs that provide predictable income [17].
Delegating with confidence using automation
Start with outsourced or freelance help before building a full team [16]. Essential early hires include a bookkeeper, practice manager, and patient navigator [4]. Automation tools can handle routine tasks—wearable devices automatically sync biometrics into patient portals [18], whereas AI-powered systems can draft patient follow-ups and generate summaries based on care plans [19].
Tracking outcomes, not just hours worked
Monitor key performance indicators such as patient outcomes, satisfaction, visit frequency, and operational efficiency [17]. Track both business growth and personal energy levels [5]. Digital outcome tracking tools convert subjective results into objective insights, allowing you to demonstrate clinical success and adjust treatment plans confidently [20].
Aligning your practice with long-term goals
Structure your practice to evolve over time—many start solo, afterward expanding into hybrid or group models as demand grows [16]. Create at least three recurring or leveraged income streams for long-term stability [16]. Consider integrating shared medical appointments (SMAs), which have shown promise for treating chronic conditions while being less costly than individual appointments [14].
Conclusion
The scalability challenge in functional medicine demands a fundamental shift in how practitioners manage overwhelming data and documentation. Clearly, the 800+ biomarkers per patient represent both an opportunity and a burden when handled through conventional methods. Therefore, implementing clinical intelligence systems offers a practical solution to this data deluge while addressing the root causes of practitioner burnout.
HolistiCare and similar platforms demonstrate that technology can transform your practice operations without sacrificing care quality. Most importantly, the 15 hours saved weekly through automation allows you to focus on what matters most—patient care and strategic health planning. This time reclamation translates directly to financial benefits, considering that functional medicine practices often leave $297,000+ in revenue unclaimed due to operational inefficiencies.
The four clinical intelligence workflows—unified data workspace, AI-generated care plans, SMART task scheduling, and real-time monitoring—work together to streamline your practice. Consequently, you can evolve from data processor to Chief Health Strategist, making better use of your expertise and training.
Your functional medicine practice can thrive without burning you out. Delegating through automation, redesigning your practitioner role, and tracking meaningful outcomes instead of hours worked will establish sustainable growth. After all, helping patients achieve optimal health should not come at the cost of your own wellbeing.
The future of functional medicine lies at this intersection of clinical excellence and operational efficiency. By embracing these solutions now, you position yourself to deliver personalized care at scale—meeting the growing demand for holistic healthcare while maintaining your passion and purpose for years to come.
Key Takeaways
Functional medicine practitioners can reclaim their time and passion by leveraging clinical intelligence systems to automate overwhelming administrative tasks while maintaining personalized patient care.
• Save 15 hours weekly: AI-powered platforms reduce clinical report preparation time by 56%, cutting average prep from 180 to 80 hours while improving accuracy by 50%.
• Transform your role: Shift from data entry clerk to Chief Health Strategist by automating the analysis of 800+ biomarkers per patient through unified data workspaces.
• Implement four key workflows: Use unified patient data, AI-generated care plans, SMART task scheduling, and real-time monitoring to streamline operations without sacrificing quality.
• Address the $297K revenue gap: Most functional medicine practices leave significant Chronic Care Management revenue unclaimed due to operational inefficiencies that automation can solve.
• Build sustainable scalability: Focus on tracking patient outcomes rather than hours worked, delegate through automation, and create recurring income streams to prevent burnout.
The path to functional medicine scalability isn’t about working harder—it’s about working smarter with technology that handles data complexity while you focus on strategic health planning and meaningful patient relationships.
FAQs
Q1. How can functional medicine practitioners save time on administrative tasks? By implementing clinical intelligence systems like HolistiCare, practitioners can automate patient protocols and save approximately 15 hours per week. This includes reducing clinical report preparation time by 56% and improving accuracy by 50%.
Q2. What are the key benefits of using AI-powered platforms in functional medicine? AI-powered platforms can analyze 800+ biomarkers per patient, generate personalized holistic health plans, and automate routine communications. This allows practitioners to transition from data processors to strategic health advisors, focusing more on patient care.
Q3. How does a unified patient data workspace improve efficiency in functional medicine practices? A unified patient workspace integrates clinical data, AI interpretation, and operational workflows, creating a single authoritative record. This ensures that the right information appears at the right time, helping practitioners make better decisions and spot missing data more easily.
Q4. What strategies can functional medicine practitioners use to build a scalable practice without burnout? Practitioners can redesign their role to focus on strategic oversight, delegate tasks using automation, track patient outcomes instead of hours worked, and create multiple recurring income streams. Considering alternative models like monthly memberships or bundled programs can also provide more predictable income.
Q5. How can real-time patient monitoring benefit functional medicine practices? Real-time patient monitoring through mobile apps and wearable technology allows practitioners to stay connected with clients, track vital signs, and detect health issues early. This enables prompt care interventions, decreases unnecessary clinic visits, and provides valuable health information that patients might not report during appointments.
References
[1] – https://holisticare.io/
[2] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10879672/
[3] – https://www.rupahealth.com/post/integrating-wearable-technology-into-patient-care-a-guide-for-functional-medicine-practitioners
[4] – https://calciumhealth.com/7-strategies-for-successfully-growing-your-functional-medicine-practice/
[5] – https://growfunctionalmedicine.com/scaling-your-functional-medicine-practice-without-burnout/
[6] – https://holisticare.io/blog/biomarker-analysis/
[7] – https://curogram.com/blog/unified-data-model-for-healthcare
[8] – https://www.healthcompiler.com/ai-data-solutions-for-functional-medicine
[9] – https://www.mdpi.com/2076-3417/14/23/10899
[10] – https://www.johnsnowlabs.com/transforming-functional-medicine-with-ai-accuracy-challenges-and-future-directions-2/
[11] – https://www.renalandurologynews.com/features/intelligent-scheduling-promises-to-improve-efficiency-patient-satisfaction/
[12] – https://fullscript.com/blog/time-management-in-functional-medicine
[13] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10730976/
[14] – https://bmjopen.bmj.com/content/11/4/e048294
[15] – https://kresserinstitute.com/why-allied-practitioners-are-the-future-of-functional-medicine/
[16] – https://growfunctionalmedicine.com/how-to-structure-a-functional-medicine-practice-for-long-term-growth/
[17] – https://fullscript.com/blog/sustainable-functional-medicine-practice
[18] – https://bodysite.com/using-technology-to-automate-functional-medicine-care/
[19] – https://hub.functionalmind.ai/ai-in-functional-medicine-transforming-clinical-insight-and-workflow-efficiency/
[20] – https://www.optimantra.com/blog/tracking-functional-outcomes-with-digital-tools-a-guide-for-integrative-holistic-practices
Disclaimer
The information in this article is provided by HolistiCare for general informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. HolistiCare does not warrant or guarantee the accuracy, completeness, or usefulness of any information contained in this article. Reliance on any information provided here is solely at your own risk.
This content does not create a doctor-patient relationship. Clinical decisions should be made by qualified healthcare professionals using clinical judgment and all available patient information. If you have a medical concern, contact your healthcare provider promptly.
HolistiCare may reference biomarker roles, study examples, products, or tools. Mention of specific tests, biomarkers, therapies, or vendors is for illustrative purposes only and does not imply endorsement. HolistiCare is not responsible for the content of third party sites linked from this article, and inclusion of links does not represent an endorsement of those sites.
Use of HolistiCare software, services, or outputs should be in accordance with applicable laws, regulations, and clinical standards. Where required by law or regulation, clinical use of biomarker information should rely on validated laboratory results and regulatory approvals. HolistiCare disclaims all liability for any loss or damage that may arise from reliance on the information contained in this article.
If you are a patient, please consult your healthcare provider for advice tailored to your clinical situation. If you are a clinician considering HolistiCare for clinical use, contact our team for product specifications, regulatory status, and clinical validation documentation.


What do you think?
[…] generate approximately 50 petabytes of clinical data annually, yet an astounding 97% remains unused [1]. Furthermore, healthcare data exists in disconnected […]