Are you drowning in clinical data? A Clinical Intelligence Layer might be the solution you’ve been seeking. Modern longevity testing generates over 800+ biomarkers per patient, creating a massive data overload that traditional analysis methods simply cannot handle. While traditional Electronic Health Record (EHR) systems have improved operational efficiency, they fall significantly short when interpreting the complex biomarker panels that define today’s longevity medicine.
In fact, clinicians currently record one data point every 1.11 minutes, leading to widespread burnout. However, by implementing healthcare operational efficiency systems, practitioners can automate patient protocols and save approximately 15 hours per week. This represents a 56% reduction in preparation time, transforming your role from data entry clerk to Chief Health Strategist. Additionally, the economic return on investments in health optimization reaches 4.4 times through reduced healthcare costs and improved workforce productivity.
As the wellness and longevity sector is projected to exceed $10 trillion globally by 2030, your practice needs more than just data storage—it needs intelligent interpretation. Throughout this article, you’ll discover why forward-thinking clinics are adopting a Clinical Intelligence Layer, how it differs from traditional EHRs, and why this strategic shift is essential for scaling your practice in 2026 and beyond.
The Limits of EHRs in a Longevity-Focused Practice
Traditional Electronic Health Record (EHR) systems have become a double-edged sword for medical practices focused on longevity and health optimization. Despite their widespread adoption, these systems present substantial limitations that are increasingly apparent as medicine shifts toward preventive care models.
Why EHRs were built for sick care, not health optimization
Electronic Health Records were designed primarily for documenting illness, not for tracking wellness trajectories. The U.S. healthcare system remains fundamentally reactive—patients typically enter the system only after symptoms appear, often late in the disease curve when treatments are costlier and less effective. Consequently, adults receive merely 54% of recommended preventive services according to CDC data.
Traditional template-based EHRs actually compound these challenges through rigid, one-size-fits-all approaches that prioritize documentation over analysis. Unlike modern Clinical Intelligence systems, conventional EHRs lack the sophisticated infrastructure needed to transform biomarker data into actionable wellness protocols.
The fundamental disconnect is clear: EHRs excel at recording what happened in the past but offer minimal support for predicting and preventing future health issues—the cornerstone of any effective longevity practice.
The rise of 800+ biomarker panels and the 'PDF graveyard'
Today’s longevity clinics routinely order comprehensive testing that includes hundreds of biomarkers across multiple biological systems. Currently, some advanced testing companies analyze over 250 biomarkers with plans to expand to 800+ in the near future. Nevertheless, almost all this valuable data becomes trapped in what practitioners call the “PDF graveyard.”
This data fragmentation occurs because hospitals generate approximately 50 petabytes of clinical data annually, yet an astounding 97% remains unused [1]. Furthermore, healthcare data exists in disconnected silos:
-
Primary care notes in one system
-
Lab results in another location
-
Imaging in specialized PACS servers
-
Insurance information in separate databases [1]
Moreover, biomarker test reports often arrive via fax or as scanned documents with inconsistent file names [1]. These reports subsequently become buried among countless other files with no effective way to filter or search for them [1]. As a result, practitioners struggle to track multiple types of tests, leading to duplicate orders and missed clinical opportunities.
How documentation overload fuels practitioner burnout
The administrative burden of EHR systems has reached crisis levels among healthcare providers. Clinicians currently spend a staggering 28 hours per week on administrative duties [1], with medical staff dedicating even more time (34 hours weekly) to paperwork and bureaucratic tasks [1].
Perhaps most concerning, research demonstrates that 49% of physician time goes to EHR and administrative activities, leaving only 27% for actual patient care [1]. Beyond the office, physicians spend approximately 1.84 hours daily completing electronic health record documentation outside regular hours—adding up to 9.2 hours each week [2].
This documentation overload directly contributes to clinician burnout. Studies have found statistically significant correlations between documentation burden and two domains of clinician burnout syndrome: emotional exhaustion and depersonalization [3]. In fact, 64% of internists attribute “too many bureaucratic tasks” such as paperwork and charting as the primary cause of burnout [2].
The situation becomes especially problematic in longevity practices where practitioners must monitor hundreds of biomarkers simultaneously—an impossible task without computational assistance. Clinical Intelligence platforms like HolistiCare address this challenge by saving practitioners an average of 15 hours weekly through automating initial protocol drafts, effectively transforming the clinician from data entry clerk to chief health strategist [4].
What Clinical Intelligence Actually Means in 2026
By 2026, the evolution of healthcare technology will have shifted beyond mere data collection toward intelligent interpretation. Clinical intelligence represents a fundamental advancement in how medical data serves practitioners, particularly those in longevity and preventive medicine.
Clinical intelligence definition and core functions
Clinical intelligence is the strategic application of advanced technologies to healthcare data that enhances clinical decision-making, improves patient outcomes, and boosts operational efficiency [5]. Unlike traditional data analytics, clinical intelligence begins by gathering information from diverse sources—electronic medical records, incident reports, patient satisfaction surveys, and bedside feedback—transforming every entry and observation into valuable data points [5].
At its core, clinical intelligence employs sophisticated algorithms that sift through massive datasets to uncover actionable patterns and trends [5]. This process transforms raw clinical data into visual dashboards, timely alerts, and digestible reports that enable faster, evidence-based decisions [5]. Essentially, clinical intelligence functions as a GPS for healthcare operations—helping practitioners avoid roadblocks, improve efficiency, and maintain optimal patient care trajectories [5].
The primary functions of clinical intelligence include:
-
Early risk identification through pattern recognition
-
Real-time decision support with evidence-based insights
-
Continuous quality improvement through key metrics monitoring
-
Workflow optimization to reduce practitioner burnout
-
Compliance management across regulatory frameworks
EHR vs Clinical Intelligence: A side-by-side comparison
Traditional EHRs and clinical intelligence systems serve fundamentally different purposes. While EHRs excel at documentation and data storage, they often overlook the clinician behaviors that shape care and signal patient outcomes [6]. Clinical intelligence platforms, alternatively, integrate both patient data and clinician behaviors to provide a comprehensive view of clinical care [6].
|
Aspect |
Traditional EHR |
Clinical Intelligence |
|
Primary Function |
Data recording and storage |
Pattern recognition and interpretation |
|
Workflow Impact |
Increases documentation time (49% of physician time) |
Reduces administrative burden through automation |
|
Decision Support |
Basic alerts and limited suggestions |
Advanced pattern recognition across multiple data types |
|
Data Integration |
Siloed information requiring manual review |
Automated cross-referencing of multi-omic data |
|
Focus |
Past documentation |
Forward-looking prediction and prevention |
|
User Experience |
Often contributes to burnout |
Designed to alleviate decision fatigue |
By 2026, clinical intelligence will have moved from the “Peak of Inflated Expectations” to the early “Slope of Enlightenment” on the Gartner Hype Cycle—indicating that initial hype is giving way to practical reality [7]. The biggest advances won’t come from flashy demonstrations, but rather from practical tools embedded in clinical workflows, built by multidisciplinary teams understanding both technology and patient needs [7].
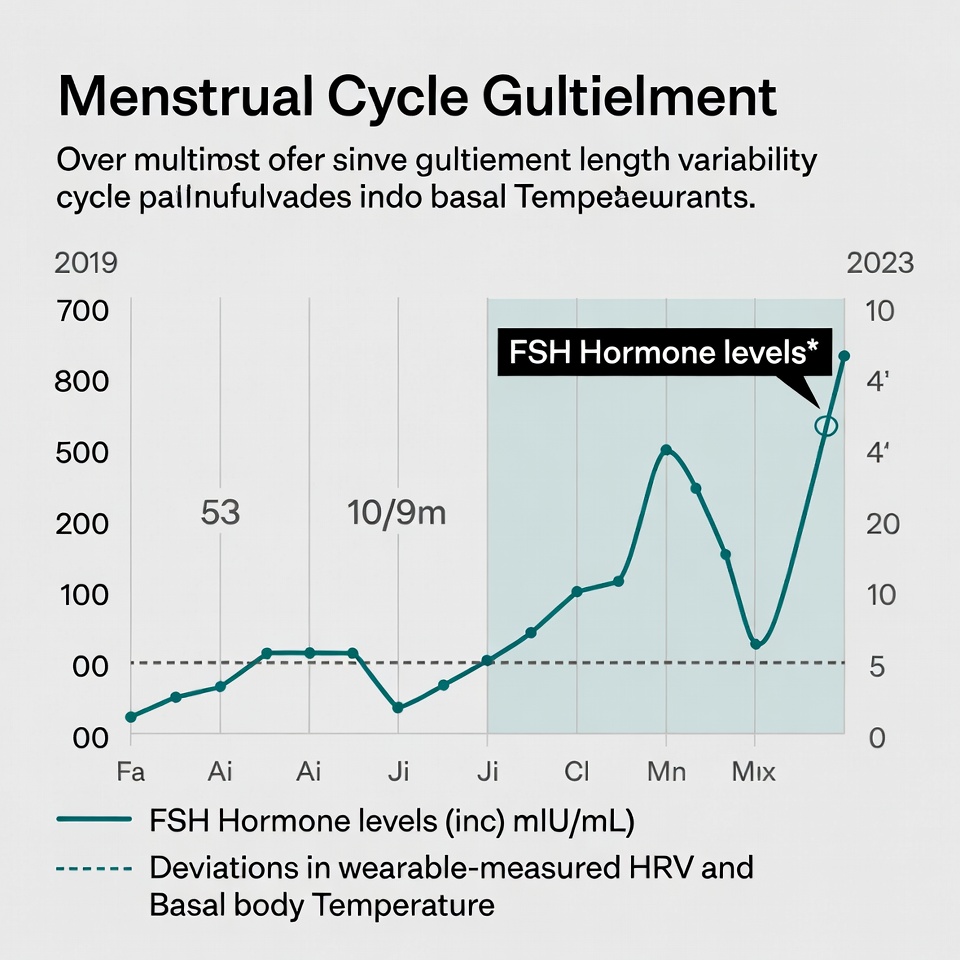
Why CI is essential for interpreting multi-omic data
The healthcare industry is experiencing unprecedented growth in multi-omic data generation—genomics, transcriptomics, proteomics, and metabolomics—creating a comprehensive biological picture that traditional analysis methods cannot process [8]. Clinical intelligence has become essential primarily because it can efficiently integrate and analyze these diverse data types to generate holistic insights [8].
For longevity clinics specifically, clinical intelligence systems shine through their ability to interpret the massive volumes of multi-omic data generated in recent decades [9]. Despite this wealth of information, practitioners still struggle to fully understand and interpret it without effective AI-based methodologies [9]. Clinical intelligence platforms address this gap by implementing advanced AI/ML approaches that identify patterns revealing predictive biomarkers and risk factors [9].
By late 2026, we’ll witness a shift from narrow, single-purpose AI tools to agentic systems that orchestrate complex clinical workflows [7]. These systems will integrate multimodal data, track patient progress, and proactively coordinate care with clinicians in the loop [7]. This advancement will be particularly crucial as AI-enabled clinical decision support systems gain accelerated adoption due to their proven ability to enhance diagnostic precision and personalize therapeutic recommendations [10].
The clinical intelligence layer truly distinguishes itself through auto-normalization capabilities—standardizing lab units, aligning reference ranges, and identifying patterns across blood markers, genetics, and microbiome data that would be impossible for humans to detect manually. Through these capabilities, clinical intelligence transforms practitioners from data entry clerks into true health strategists, allowing them to focus on developing personalized patient protocols instead of drowning in documentation.
Inside the Clinical Intelligence Layer: How It Works
The modern clinical intelligence layer acts as the brain behind effective health optimization practices, transforming raw data into actionable insights through several key mechanisms.
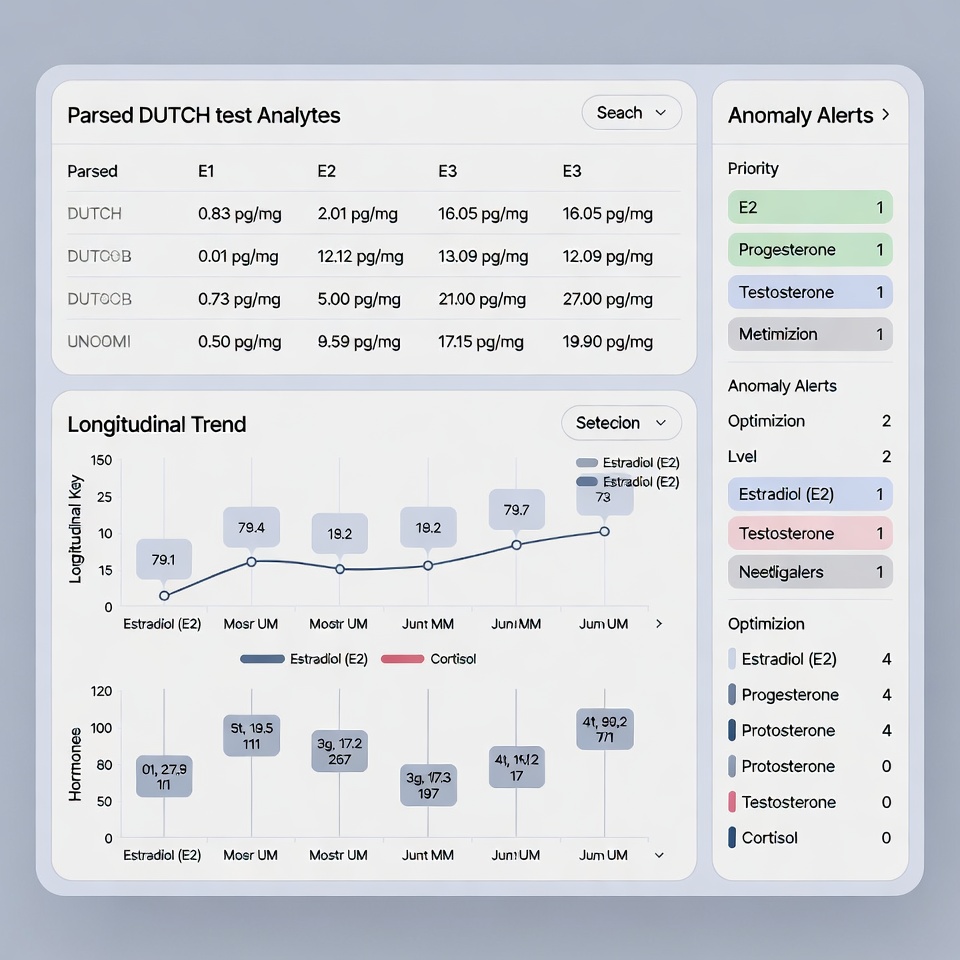
Auto-normalization of lab units and reference ranges
One of the primary challenges in clinical data interpretation is the inconsistency in laboratory units and reference ranges. Laboratory result interpretation is often hindered by variability across different institutions and analytes, delaying clinical decisions and increasing cognitive effort [11]. Clinical intelligence platforms address this through automated unit normalization—converting heterogeneous values into standardized formats.
Advanced normalization methods transform laboratory values into dimensionless scores using simple rescaling formulas based on the reference range. By converting values to a 0 to 1 or -1 to 1 scale, this approach allows intuitive assessment and direct comparison across different tests, regardless of their original units [11]. First, the system standardizes heterogeneous unit expressions into valid UCUM codes, thereafter harmonizing them to designated reference units within LOINC groups [12].
Pattern recognition across blood, genetics, and microbiome
Beyond normalizing individual values, clinical intelligence identifies meaningful patterns across multiple data types. Instead of presenting clinicians with isolated abnormal results, the system identifies clinically meaningful patterns and ranks them by probable impact [13].
For instance, a mild ALT elevation combined with high GGT and recent statin initiation might surface as a prioritized ‘hepatic stress’ cluster with suggested immediate checks, monitoring cadence, and confidence notes [13]. This multi-omic approach is vital since microbiome analysis also presents challenges, including high host DNA background and multiple contamination sources [14].
Automated biomarker interpretation at scale
Biomarker discovery automation leverages robotics and digital technologies to optimize operations and accelerate candidate identification [15]. After automatically capturing data, the system ingests both assay-specific output and rich metadata such as sample IDs, species, reagents, and timepoints in real time [16].
This automation allows vast amounts of data to be imported and transformed faster, scaling with growing data sources and formats, while minimizing manual entry mistakes [16]. The platform applies out-of-the-box assay-specific workflows to analyze data consistently, delivering reliable, reproducible results [16].
HolistiCare as a central intelligence layer
HolistiCare exemplifies this approach, functioning as a central intelligence layer that ingests multi-vendor data, standardizes it into a canonical model, and applies transparent interpretation [13]. The platform supports:
-
Auto-Normalization: Automatically handling unit conversions and mapping vendor-specific reference ranges to age/sex-specific intervals [13]
-
Legacy Data Import: Supporting bulk historic imports, allowing backfill of patient histories for immediate trend analysis [13]
-
Multi-Omics Support: Consolidating clinical labs, genomics, microbiome, and lifestyle data in one view [13]
This automation shifts the practitioner’s focus from data management to strategic interpretation and care planning, reducing the time needed to produce clinical reports by 56%—cutting average preparation time from 180 hours to just 80 hours [17].
The Operational ROI: Time, Burnout, and Patient Outcomes
Implementing a clinical intelligence layer delivers immediate operational benefits that transform how practitioners manage their time and care for patients.
The 15-hour weekly win for practitioners
Clinicians currently spend approximately 28 hours weekly on administrative duties, with medical staff dedicating even more time (34 hours) to paperwork and bureaucratic tasks [1]. Through clinical intelligence automation, practitioners gain back approximately 15 hours every week [1]. This represents a 56% reduction in preparation time, cutting average report creation from 180 hours to just 80 hours [1]. Notably, physicians spend 49% of their time on EHR and administrative activities, leaving only 27% for actual patient care [1].
From data entry clerk to Chief Health Strategist
The transformation goes beyond time savings. Clinical intelligence platforms enable practitioners to transition from data processors to strategic health advisors. Currently, physicians dedicate about 16 minutes per patient on EHR tasks—for a primary care doctor seeing 20 patients daily, that amounts to 5+ hours of charting plus 1-2 additional hours at night [18]. AI automation in documentation saves up to two hours per provider daily [1], allowing them to refocus on developing personalized treatment plans rather than drowning in documentation.
Improved patient retention and satisfaction
Patient retention directly impacts both growth and profitability. High attrition rates result in substantial financial losses and increased operational costs as providers must continually invest in acquiring new patients [4]. Clinical intelligence platforms enhance retention by identifying at-risk patients through predictive analytics, enabling early interventions [4]. Furthermore, these systems analyze patient feedback to pinpoint major satisfaction drivers [4].
Reduced decision fatigue and faster protocol creation
Physicians make an average of 13.4 clinically relevant decisions during each patient encounter [19]. This continuous decision-making leads to decision fatigue—a state of mental overload that impairs judgment and increases error risk [20]. Clinical intelligence platforms reduce this burden by automating routine decisions, providing evidence-based suggestions, and streamlining protocol creation. Therefore, practitioners can focus their cognitive resources on complex clinical reasoning rather than administrative tasks.
Why Smart Clinics Are Making the Shift Now
Forward-thinking medical practices are rapidly adopting clinical intelligence layers as essential components of their technology infrastructure. This strategic shift represents a fundamental evolution in how longevity clinics handle patient data and care delivery.
Longevity Clinic Tech Stack: What's changing in 2026
In 2026, longevity medicine has matured beyond elite biohackers into evidence-based practices accessible to broader populations [21]. Comprehensive metabolic monitoring through continuous glucose monitors has gone mainstream, with 76% of doctors now recommending them to patients [21]. Furthermore, clinical intelligence is becoming a strategic necessity as healthcare undergoes massive digital transformation [5].
Medical practice scalability through automation
Automation represents a USD 150 billion opportunity for operational improvement in healthcare [22]. Although payers have the most to gain, providers benefit substantially from automating repetitive tasks that currently consume their practice time. By 2025-2026, over 70% of healthcare executives are prioritizing tech-enabled models to meet rising demands [23].
How early adopters are gaining a competitive advantage
Early AI adopters are creating a widening performance gap in healthcare delivery [24]. Those who implement clinical intelligence first report tangible results: improved data accuracy (70%) and streamlined data collection (61%) [25]. Most tellingly, 73% of AI users report that the technology has met or exceeded expectations [25].
The message is clear—organizations that delay implementation risk marginalization even if they currently maintain strong financial performance [24]. Forward-thinking health systems understand that clinical intelligence isn’t just an opportunity but a competitive necessity [24].
Conclusion
As healthcare evolves toward preventive models, traditional EHRs simply cannot handle the complexity of modern longevity medicine. These systems, designed primarily for documenting illness rather than optimizing health, fail to interpret the 800+ biomarkers now standard in comprehensive testing. Consequently, clinicians find themselves recording data points every 1.11 minutes while valuable insights remain trapped in the “PDF graveyard.”
Clinical Intelligence represents a paradigm shift rather than merely an incremental improvement. Unlike conventional EHRs, these platforms automatically normalize lab units, identify patterns across blood markers, genetics, and microbiome data, while transforming raw information into actionable protocols. Therefore, platforms like HolistiCare function as central intelligence layers that ingest multi-vendor data and apply transparent interpretation at scale.
The operational benefits prove substantial and immediate. Through automation, practitioners gain back approximately 15 hours weekly—time previously lost to administrative tasks. This 56% reduction in preparation time allows you to transition from data entry clerk to Chief Health Strategist. Additionally, the improved patient experience translates directly to better retention rates and practice growth.
Smart clinics recognize that waiting is no longer an option. Early adopters already report improved data accuracy, streamlined collection processes, and enhanced clinical outcomes. Though traditional EHRs served their purpose in digitizing medical records, Clinical Intelligence now offers what forward-thinking practices truly need—not just data storage but intelligent interpretation that scales with your practice.
The future belongs to clinicians who can focus their expertise on developing personalized treatment plans instead of drowning in documentation. After all, your patients didn’t come to you for data entry skills but for your clinical judgment. Clinical Intelligence systems finally enable you to deliver that expertise efficiently and effectively, positioning your practice for success in 2026 and beyond.
Key Takeaways
Smart clinics are revolutionizing healthcare delivery by implementing Clinical Intelligence layers that transform overwhelming biomarker data into actionable insights, enabling practitioners to focus on strategic patient care rather than administrative burden.
• Clinical Intelligence saves 15 hours weekly by automating data interpretation and protocol creation, reducing preparation time by 56% from traditional EHR workflows.
• Traditional EHRs fail longevity medicine – designed for sick care documentation, they can’t interpret 800+ biomarker panels that define modern preventive healthcare.
• Auto-normalization transforms practice efficiency by standardizing lab units, identifying patterns across genetics/microbiome data, and eliminating the “PDF graveyard” problem.
• Early adopters gain a competitive advantage with 73% reporting AI exceeded expectations, while delayed implementation risks practice marginalization in the evolving healthcare landscape.
• Practitioners become Chief Health Strategists instead of data entry clerks, transitioning from 49% administrative time to strategic patient care and personalized protocol development.
The shift from reactive documentation to proactive intelligence represents healthcare’s future – where technology amplifies clinical expertise rather than drowning it in paperwork, ultimately improving both practitioner satisfaction and patient outcomes.
FAQs
Q1. What is a Clinical Intelligence Layer, and why is it important for smart clinics? A Clinical Intelligence Layer is an advanced technology system that interprets complex medical data, identifies patterns, and provides actionable insights. It’s crucial for smart clinics because it helps manage the overwhelming amount of biomarker data in modern preventive medicine, improving efficiency and patient care.
Q2. How does Clinical Intelligence differ from traditional Electronic Health Records (EHRs)? While EHRs primarily focus on data storage and documentation, Clinical Intelligence systems go further by automatically interpreting data, recognizing patterns across multiple biomarkers, and providing decision support. This allows practitioners to focus more on strategic patient care rather than administrative tasks.
Q3. What are the main benefits of implementing a Clinical Intelligence Layer? The key benefits include saving practitioners about 15 hours per week through automation, reducing burnout by minimizing administrative tasks, improving patient retention and satisfaction, and enabling faster, more accurate protocol creation based on comprehensive data analysis.
Q4. How does Clinical Intelligence help in interpreting multi-omic data? Clinical Intelligence systems can efficiently integrate and analyze diverse data types such as genomics, proteomics, and metabolomics. They use advanced AI/ML approaches to identify patterns, reveal predictive biomarkers, and generate holistic insights that would be impossible for humans to detect manually.
Q5. Why are smart clinics adopting Clinical Intelligence now? Smart clinics are adopting Clinical Intelligence now because it offers a competitive advantage in the rapidly evolving healthcare landscape. Early adopters report improved data accuracy, streamlined processes, and enhanced clinical outcomes. As healthcare undergoes digital transformation, Clinical Intelligence is becoming a strategic necessity for scaling practices and meeting rising demands.
References
[1] – https://holisticare.io/blog/functional-medicine-scalability-roi/
[2] – https://physiciansangels.com/learning-center/documentation-overload-and-internist-burnout/
[3] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9581587/
[4] – https://clarifyhealth.com/insights/blog/enhancing-patient-retention-through-predictive-analytics/
[5] – https://pristacorp.com/insights/what-is-clinical-intelligence-benefits-importance/
[6] – https://www.nature.com/articles/s44401-025-00040-5
[7] – https://www.massgeneralbrigham.org/en/about/newsroom/articles/2026-predictions-about-artificial-intelligence
[8] – https://www.annualreviews.org/content/journals/10.1146/annurev-biodatasci-102523-103801
[9] – https://www.futuremedicine.com/articles/advancing-precision-medicine-with-ai-for-integrated-multi-omics-and-clinical-data-analysis
[10] – https://www.sas.com/en_us/news/press-releases/2025/december/health-life-sciences-2026-predictions.html
[11] – https://pmc.ncbi.nlm.nih.gov/articles/PMC12168664/
[12] – https://www.sciencedirect.com/science/article/pii/S138650562500348X
[13] – https://holisticare.io/features/clinical-data-analysis-software/
[14] – https://academic.oup.com/bib/article/26/2/bbaf176/8118856
[15] – https://www.genedata.com/resources/learn/details/blog/how-is-automation-transforming-biomarker-discovery
[16] – https://www.drugdiscoverytrends.com/finding-signals-in-the-storm-automation-in-biomarker-discovery/
[17] – https://holisticare.io/blog/longevity-medicine-2026-strategy/
[18] – https://verinoteai.com/blog/reduce-charting-time-for-doctors-2026-guide/
[19] – https://www.aafp.org/pubs/fpm/blogs/inpractice/entry/decision-fatigue.html
[20] – https://www.ama-assn.org/public-health/behavioral-health/what-doctors-wish-patients-knew-about-decision-fatigue
[21] – https://honehealth.com/edge/longevity-trends/?srsltid=AfmBOoo_RxsgO9Yy2WD6Yg9CJDCSTbepcoOx1xKMp7OEN2ZVFC0j_LDi
[22] – https://www.mckinsey.com/capabilities/operations/our-insights/making-healthcare-more-affordable-through-scalable-automation
[23] – https://www.notablehealth.com/blog/how-automation-improves-patient-outcomes-at-scale
[24] – https://hmacademy.com/insights/AI-Catalyst/artificial-intelligence/ai-in-healthcare-from-strategic-priority-to-competitive-necessity
[25] – https://pharmaphorum.com/sales-marketing/ai-imperative-establishing-standard-modern-clinical-research
Disclaimer
The information in this article is provided by HolistiCare for general informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. HolistiCare does not warrant or guarantee the accuracy, completeness, or usefulness of any information contained in this article. Reliance on any information provided here is solely at your own risk.
This content does not create a doctor-patient relationship. Clinical decisions should be made by qualified healthcare professionals using clinical judgment and all available patient information. If you have a medical concern, contact your healthcare provider promptly.
HolistiCare may reference biomarker roles, study examples, products, or tools. Mention of specific tests, biomarkers, therapies, or vendors is for illustrative purposes only and does not imply endorsement. HolistiCare is not responsible for the content of third party sites linked from this article, and inclusion of links does not represent an endorsement of those sites.
Use of HolistiCare software, services, or outputs should be in accordance with applicable laws, regulations, and clinical standards. Where required by law or regulation, clinical use of biomarker information should rely on validated laboratory results and regulatory approvals. HolistiCare disclaims all liability for any loss or damage that may arise from reliance on the information contained in this article.
If you are a patient, please consult your healthcare provider for advice tailored to your clinical situation. If you are a clinician considering HolistiCare for clinical use, contact our team for product specifications, regulatory status, and clinical validation documentation.


What do you think?
[…] Electronic Health Records (EHRs) were designed primarily for documentation, billing support, and regulatory compliance, not for real-time intelligence or cross-system data exchange. […]