Did you know that losing a patient can cost a clinic between $100,000 and $300,000 in lifetime value, depending on the services offered and the length of retention? Patient retention in longevity clinics is not just about maintaining relationships; it’s a crucial economic necessity.
Interestingly, acquiring new patients can cost five to twenty-five times more than retaining existing ones, with costs varying by practice. This reality is particularly challenging in preventative medicine, where patients often don’t immediately notice the results of their treatments. Factors such as cost and access also contribute to discontinued care.
There is a solution to the patient retention challenge in longevity clinics. By implementing biological age tracking with metrics like DunedinPACE—a key performance indicator that measures the pace of aging—your clinic can provide patients with tangible results within three to six months, although the frequency of testing depends on the specific metric used. This approach not only enhances the longevity of the patient lifecycle but also transforms your functional medicine business model.
Additionally, many functional medicine practices leave between $150,000 and $350,000 in Chronic Care Management revenue unclaimed due to operational inefficiencies. By utilizing the right clinical intelligence systems to manage the overwhelming number of 800+ biomarkers, you can turn this data into meaningful insights for patients while achieving a 4.4x return on investment in preventative health. Let’s explore how you can leverage biological age tracking for better patient outcomes and significant practice growth.
Why Biological Age is the Ultimate Longevity KPI
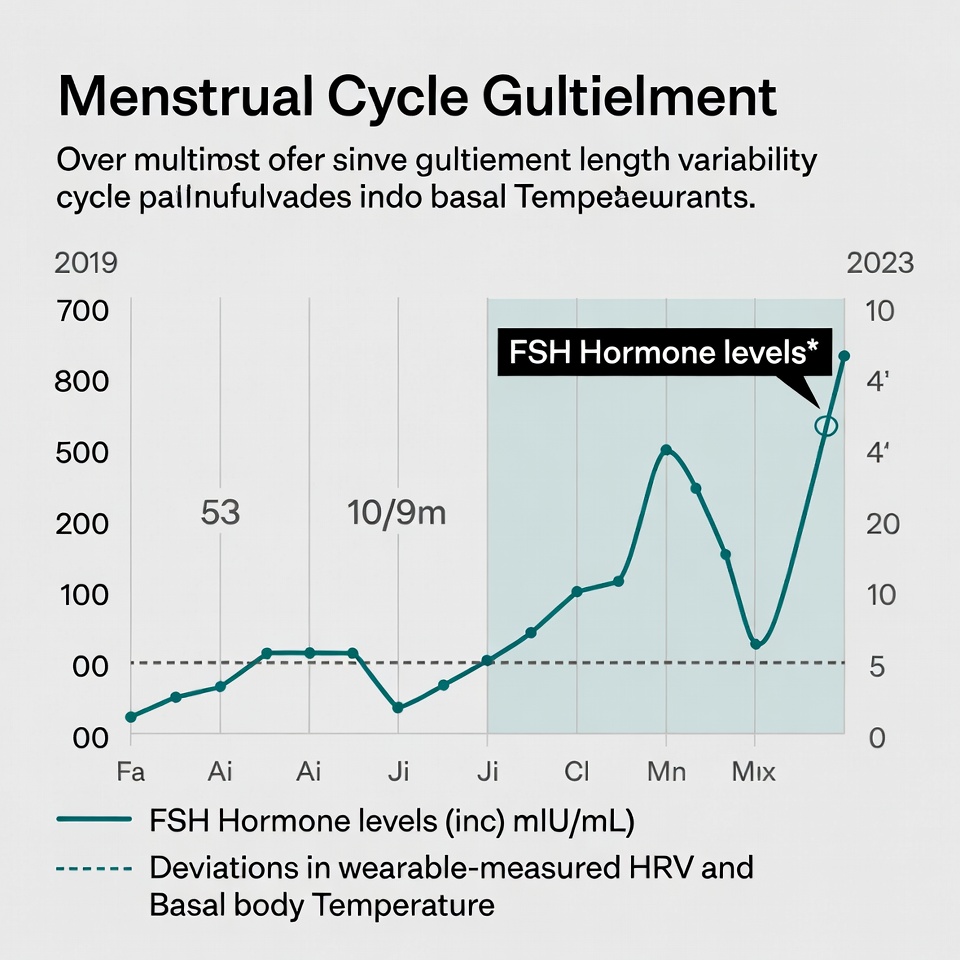
Chronological age is merely a number. Biological age, on the other hand, reveals what’s actually happening inside your body. For longevity clinics, this distinction creates a fundamental opportunity: while patients can’t immediately “feel” preventive interventions, they can see their biological age improve—creating a measurable win that keeps them engaged in their health journey.
Beyond the 'Normal' Range: Why patients need optimization metrics
Traditional lab results often label values as either “normal” or “abnormal,” a binary system that fails to capture the nuances of optimal health. This approach creates a critical challenge for patient retention for longevity clinics—when everything looks “normal,” patients question why they should continue treatment.
Biological age metrics solve this dilemma by shifting the conversation from “normal” to “optimal.” Unlike standard reference ranges that include both healthy and unhealthy individuals, biological age provides a clear target: becoming younger at the cellular level.
This matters enormously because chronological age is the leading risk factor for virtually all chronic diseases [1]. Nonetheless, people of identical chronological age can show vast differences in overall health [2]. Some develop multiple chronic conditions by midlife, while others maintain excellent health into their 70s and beyond [2].
Consequently, longevity clinics need metrics that capture these differences. When patients see their biological age exceed their chronological age—what researchers call “epigenetic age acceleration”—they understand immediately that something needs to change [1]. This acceleration is associated with increased risk of:
For this reason, tracking biological age becomes the cornerstone of a functional medicine business model that actually retains patients. When patients see their biological age decrease over time, they have tangible proof your interventions are working, long before disease symptoms would have appeared.
DunedinPACE: Measuring the pace of aging in months, not years
Among biological age measures, DunedinPACE stands out as a revolutionary advancement specifically designed to function as a “speedometer for aging” [3].
Developed using data from participants tracked from ages 26 to 45, DunedinPACE measures something fundamentally different from other aging clocks [3]. Rather than estimating how old someone is, it measures how quickly they’re currently aging [3]. This distinction makes it especially valuable for the longevity patient lifecycle.
What makes DunedinPACE particularly powerful for clinic economics? Six key design advantages:
-
It’s derived from longitudinal data with tests spaced 5 years apart, preventing short-term illness from skewing results [3]
-
It was developed using healthy adults before disease onset [3]
-
It compares individuals of the same chronological age, avoiding generational bias [3]
-
It avoids “survival bias” by tracking midlife adults [3]
-
It achieves exceptional test-retest reliability of over .90 [3]
-
It’s specifically designed to be responsive to interventions [3]
Furthermore, DunedinPACE shows strong associations with morbidity, disability, and mortality [4] while offering valuable predictive information beyond other measures [4]. In validation studies, individuals with faster DunedinPACE were at increased risk for chronic disease, disability, and death [3].
Given these capabilities, DunedinPACE offers an ideal KPI for both patient health outcomes and practice economics. Since it’s specifically designed to detect change, it excels at showing patients their progress during the critical early months of treatment—precisely when they’re deciding whether to continue with your clinic.
By implementing biological age tracking through metrics like DunedinPACE, your clinic gives patients something most healthcare providers cannot: visible proof they’re getting biologically younger. This creates a powerful retention engine that translates directly into clinical and economic outcomes.
The Psychology of Progress: Turning Data into 'Aha!' Moments
Visualizing progress creates powerful psychological moments of insight. When patients can see their health improving through data, abstract concepts become tangible reality. For longevity clinics, this visualization capability transforms patient retention from a challenge into a competitive advantage.
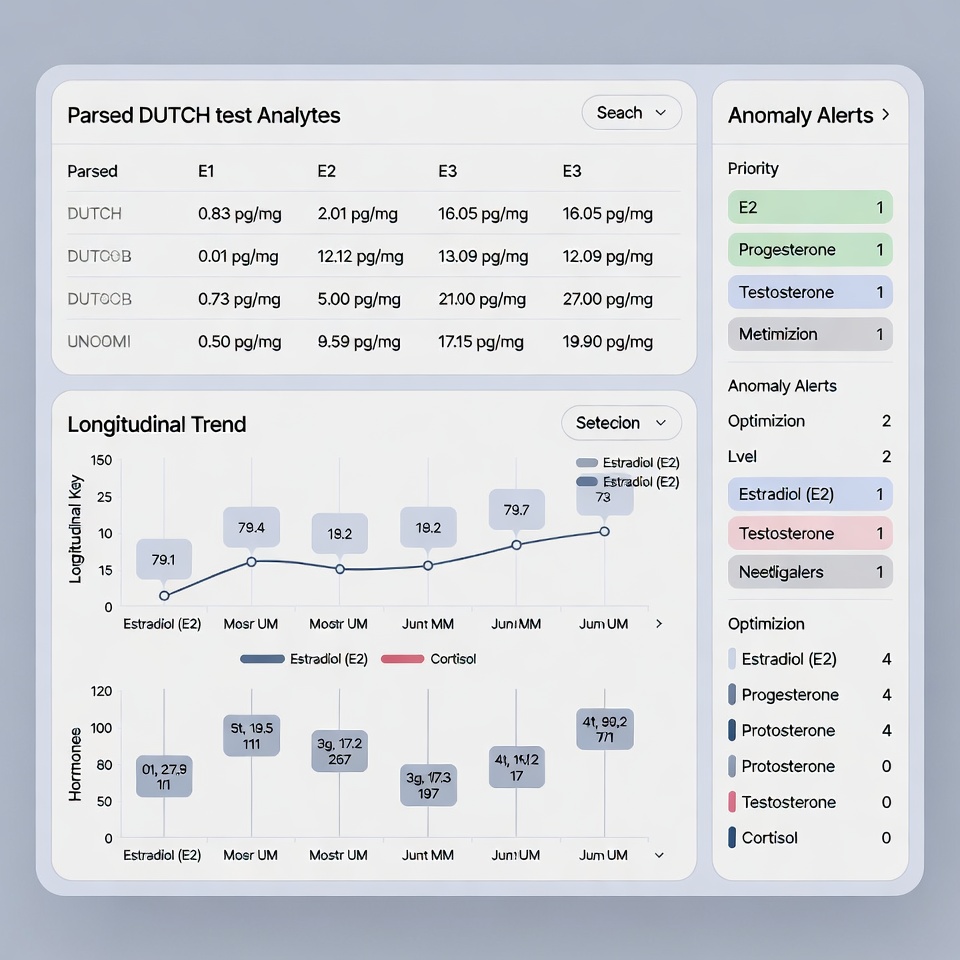
Using 800+ biomarkers to tell a compelling health story
The human body generates an overwhelming amount of biological data. A typical longevity client undergoes multiple advanced tests, including genomic sequencing, multi-omics profiling, advanced imaging, full body scans, immune system assessments, microbiome analyzes, and epigenetic testing [5]. This deep phenotyping reveals aging patterns typically missed in conventional healthcare settings.
Nevertheless, this data abundance creates a paradox: How can you transform hundreds of data points into a compelling narrative that patients actually understand? The answer lies in sophisticated data visualization.
Effective data visualization reduces complexity by leveraging humans’ powerful ability to visually perceive differences in sizes, shapes, colors, and spatial positions [2]. Indeed, visualization techniques such as bubble charts, parallel coordinates line graphs, box plots, and alluvial flow diagrams excel at revealing patterns in multidimensional datasets [6].
The most successful visualizations for health data incorporate:
-
Color (used in 77% of effective health visualizations) [2]
-
Numerical context (included in 88% of visualizations) [2]
-
Easily understood symbols like traffic light schemes [2]
-
Interactive elements allowing patients to zoom from overviews to detailed information [7]
Above all, these visualizations must tell a story. Patients need to see relationships between their actions and outcomes—the foundation of the “Aha!” moment that drives retention for longevity clinics.
How measurable results drive long-term patient adherence
Patient non-adherence remains one of healthcare’s most persistent challenges. Studies reveal that up to 50–67% of patients skip medication doses, primarily due to forgetfulness, disrupted routines, or being busy [8]. In contrast, when patients can directly connect their actions to measurable improvements, adherence rates improve dramatically.
Accordingly, visualization of progress serves as a powerful adherence driver. When patients see their biological age markers improving, they experience increased self-efficacy—a key psychological factor in long-term health engagement [9]. This visual confirmation transforms abstract preventative care into concrete evidence of success.
In fact, a condition management project implementing personalized communications based on behavioral science can increase Patient Activation Measure (PAM) scores by 20%+ in some interventions. Furthermore, such approaches can significantly improve patient enrollment rates [10].
The financial implications are substantial. For longevity clinics, improved adherence creates a virtuous economic cycle:
First, patients stay engaged longer when they can track their progress through visualized biomarkers.
Second, these engaged patients achieve better outcomes as they maintain their protocols.
Third, improved outcomes generate positive word-of-mouth, reducing patient acquisition costs.
Fourth, reduced acquisition costs combined with longer patient relationships dramatically improve lifetime value.
The connection between data visualization and economic outcomes becomes clearer when examining how patients interact with their health information. Studies show patients strongly prefer visualizations that provide context, use familiar colors/symbols, and clearly display goal ranges [2]. Equally important, visualizations that include goal ranges produce higher comprehension levels and decreased negative reactions to borderline results [2].
Ultimately, when individuals become deeply involved in understanding and managing their own biology through visualized data, adherence improves substantially [5]. Lifestyle modifications—still the most robust interventions for healthy aging—become normalized rather than burdensome. Through this mechanism, the psychological power of seeing progress translates directly into economic results for longevity clinics committed to patient retention.
The 4.4x ROI: The Math Behind Preventative Health
Prevention isn’t just better medicine—it’s better business. The economics of preventative health present a compelling case for longevity clinics seeking sustainable growth. Studies reveal that for every dollar invested in healthy aging initiatives, three dollars return to society through economic and healthcare benefits [11]. This return magnifies even further when implemented strategically within a clinical setting.
Preventative services remain substantially underutilized despite their proven effectiveness. According to CDC data, approximately 40–50% of adults receive routine immunizations for influenza, and around 70–80% are screened for tobacco use with cessation assistance [12]. This gap represents both a health crisis and a significant economic opportunity for forward-thinking longevity clinics.
Bridging the $297,000 revenue gap in Chronic Care Management
Chronic Care Management (CCM) represents one of the most successful value-based care programs created by Medicare, yet many longevity clinics leave substantial revenue unclaimed. With just 300 enrolled patients, a practice can generate approximately $180,000–$360,000 in additional fee-for-service payments annually, based on $50–100 per patient per month [13]. Moreover, practices enrolling 250 patients in a comprehensive program could see between $150,000–$352,500 in direct revenue each year [14].
The financial impact extends beyond direct billing. CCM programs create multiple revenue streams that collectively bridge the typical $297,000 gap:
-
Fee-for-service monthly payments – Recurring revenue from enrolled patients
-
Medicare Shared Savings Program enhancements – CCM patients experience 5–13% fewer ED admissions and hospital readmissions [13]
-
Quality payment bonuses – CCM programs can boost MIPS scores, with medians around 84–90 and some achieving a perfect 100 [13]
-
Reduced patient leakage – Keeping high-value specialty care in-network
-
Increased E&M encounters – Analysis shows CCM programs boost average E&M visits by 8% [13]
Implementing CCM requires appropriate staffing. Research indicates that a practice would need to enroll approximately 100–150 Medicare patients to recoup the salary and overhead costs of hiring a full-time nurse for Chronic Care Management services [14].
Reducing the cost per interaction through Clinical Intelligence
Clinical Intelligence systems dramatically reduce costs while maintaining quality. A groundbreaking study identified that using AI can reduce costs by 10–50% in healthcare tasks when operating efficiently [15]. This approach involves grouping up to 50 clinical tasks—from matching patients for clinical trials to identifying candidates for preventive screenings—without significant accuracy loss [16].
Companies implementing comprehensive preventative health programs report extraordinary economic outcomes, including:
-
40–50% reductions in healthcare utilization through prevention [3]
-
Early detection in preventative health programs results in 50–70% lower treatment costs[3]
-
Early disease detection can yield up to nine times ROI in productivity recovery in some programs[3]
As a matter of fact, organizations with strong health cultures experience a 21% boost in overall productivity [3]. Given these points, the economic case becomes clear: investing in a Clinical Intelligence system to manage biomarker analysis and patient monitoring delivers substantial ROI through both direct revenue generation and operational cost reduction.
When implemented strategically, preventative health programs have demonstrated returns of up to 13:1 over a ten-year horizon in some studies, typically 3:1–6:1 overall [3], making them among the most profitable investments a longevity clinic can make.
Implementing a High-Retention Workflow with HolistiCare
Effective implementation separates successful longevity clinics from those struggling with retention. Once you’ve established biological age as your key performance indicator, the next step involves creating workflows that consistently deliver results while minimizing administrative burden. HolistiCare provides this infrastructure through automated monitoring and intelligent task management.
Automated check-ins and real-time monitoring
HolistiCare streamlines patient monitoring through brief, validated check-ins delivered via app, SMS, or email based on patient preference [1]. These check-ins take less than two minutes to complete yet provide crucial data points that feed into a comprehensive patient timeline [1]. Unlike traditional follow-up systems that overwhelm both patients and staff, HolistiCare emphasizes signal detection rather than exhaustive surveys.
The system’s pattern recognition capabilities identify deteriorations and alert your care team with prioritized context for faster triage [1]. This approach respects patient burden by automatically adjusting check-in frequency based on prior responses and adherence patterns. Stable patients receive fewer check-ins, while those showing missed checks or worsening scores generate notifications for human intervention [1].
This adaptive approach maintains safety while preserving clinic resources. The system combines patient-reported outcomes with wearable and home device data to create a multi-source signal [1]. For example, a heart failure monitoring program might pair daily weight checks with symptom reporting to detect fluid retention early.
SMART task scheduling for real-world adherence
When implementing longevity protocols, patient adherence often determines success or failure. Studies show 63.2% of patients skip medication doses primarily due to forgetfulness, disrupted routines, or being busy [17]. HolistiCare addresses these challenges through SMART (Specific, Measurable, Achievable, Relevant, Time-bound) task scheduling.
The platform creates structured triage flows that streamline response and provide an auditable trail for quality review [1]. Every alert generates a task with a suggested action and documented resolution once completed. Clinics define which responses generate automated messages, require clinician review, or need emergency instructions [1].
For programs with high check-in volumes, intelligent rules can batch non-urgent issues into daily summaries while immediately flagging critical events [1]. This reduces alert fatigue while ensuring urgent problems receive prompt attention. Program managers can view cohort dashboards showing completion rates, trends in symptom burden, and escalation frequencies [1].
These features collectively save practitioners up to 15 hours weekly, allowing them to shift from administrative tasks to becoming Chief Health Strategists for their patients. Most importantly, this comprehensive monitoring system creates the foundation for the 4.4x ROI discussed earlier by ensuring patients stay engaged with their protocols throughout the longevity patient lifecycle.
Conclusion: Building a Scalable Practice That Values Outcomes
Patient retention emerges as both a critical challenge and a tremendous opportunity for longevity clinics. Throughout this article, we’ve seen how biological age tracking creates the measurable results patients need to stay engaged with preventative protocols they can’t immediately “feel” working. DunedinPACE specifically offers an ideal solution as it measures the pace of aging, providing tangible evidence of improvement every 3-6 months.
The economics clearly support this approach. Your clinic can achieve that powerful 4.4x ROI while simultaneously bridging the $297,000 revenue gap that many functional medicine practices unknowingly leave unclaimed. Additionally, Clinical Intelligence systems significantly reduce costs by managing the overwhelming 800+ biomarkers that come with comprehensive longevity testing.
Psychological factors also play a crucial role. Patients who see their biological age decrease experience powerful “Aha!” moments that drive long-term adherence. This visualization of progress transforms abstract preventative care into concrete evidence of success, creating a virtuous cycle where better outcomes generate word-of-mouth referrals that reduce acquisition costs.
Therefore, implementing systems like HolistiCare becomes essential for sustained practice growth. Automated check-ins and SMART task scheduling save practitioners up to 15 hours weekly while ensuring patients stay engaged throughout their longevity journey. This time savings allows you to shift from administrative tasks to becoming a true Chief Health Strategist for your patients.
The path forward is clear. Biological age tracking isn’t just about better medicine—it’s better business. By providing patients with visible proof they’re getting younger at the cellular level, you create a retention engine that other clinics simply cannot match. Most importantly, this approach aligns economic incentives with optimal patient care, allowing you to build a thriving practice while genuinely improving lives through preventative health.
Key Takeaways
Longevity clinics can transform patient retention challenges into substantial revenue growth by implementing biological age tracking and data-driven workflows that provide measurable results patients can see and understand.
• Biological age tracking drives retention: DunedinPACE measures aging pace in months, giving patients tangible proof of improvement every 3-6 months when they can’t “feel” preventative treatments working.
• Data visualization creates psychological wins: Converting 800+ biomarkers into compelling visual stories generates powerful “Aha!” moments that dramatically improve long-term patient adherence.
• Preventative health delivers 4.4x ROI: Strategic implementation bridges the $297,000 revenue gap in Chronic Care Management while reducing operational costs through Clinical Intelligence systems.
• Automated workflows save 15 hours weekly: SMART task scheduling and real-time monitoring through platforms like HolistiCare streamline operations while maintaining high-quality patient engagement.
• Retention costs 5x less than acquisition: Losing one patient can cost up to $200,000 in lifetime value, making retention the most profitable investment for sustainable practice growth.
The key insight: When patients see their biological age decreasing, they have undeniable proof your interventions work—creating a retention engine that aligns economic success with optimal patient outcomes in preventative medicine.
FAQs
Q1. What is biological age and why is it important for longevity clinics? Biological age reflects the actual state of your body’s health, as opposed to chronological age. It’s crucial for longevity clinics because it provides measurable evidence of health improvements, keeping patients engaged in their preventative health journey even when they can’t immediately feel the effects of treatments.
Q2. How does DunedinPACE differ from other biological age measurements? DunedinPACE is designed as a “speedometer for aging,” measuring how quickly a person is currently aging rather than estimating their age. It’s particularly valuable because it’s responsive to interventions, has high test-retest reliability, and is derived from longitudinal data of healthy adults before disease onset.
Q3. What is the economic benefit of implementing preventative health programs in longevity clinics? Preventative health programs can yield a 4.4x return on investment (ROI) for longevity clinics. This includes bridging a $297,000 revenue gap in Chronic Care Management, reducing operational costs through Clinical Intelligence systems, and improving patient retention, which is five times less expensive than acquiring new patients.
Q4. How can data visualization improve patient adherence to longevity protocols? Effective data visualization transforms complex biomarker data into compelling visual stories that patients can easily understand. This creates powerful “Aha!” moments, showing patients the direct connection between their actions and health improvements, which significantly boosts long-term adherence to longevity protocols.
Q5. What role does automated monitoring play in improving patient retention for longevity clinics? Automated monitoring systems, like those offered by HolistiCare, streamline patient check-ins and provide real-time health data. This allows for early detection of health issues, personalized care adjustments, and efficient task management for clinic staff. By ensuring consistent patient engagement and timely interventions, these systems play a crucial role in improving patient retention and outcomes.
References
[1] – https://holisticare.io/features/check-ins/
[2] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6785326/
[3] – https://www.morningstar.com/news/pr-newswire/20251201ny34139/fountain-life-redefines-employee-health-with-executive-health-program-delivering-20m-annual-roi-and-80-member-optimization-success
[4] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9777836/
[5] – https://pmc.ncbi.nlm.nih.gov/articles/PMC12606959/
[6] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9299558/
[7] – https://informatics.bmj.com/content/23/3/600
[8] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11192640/
[9] – https://healthexpertsalliance.com/the-psychology-of-longevity-why-offering-anti-aging-services-builds-emotional-loyalty/
[10] – https://www.engagys.com/insights/driving-medication-adherence-medical-device-usage-pam-scores
[11] – https://www.mckinsey.com/mhi/our-insights/the-economic-case-for-investing-in-healthy-aging-lessons-from-the-united-states
[12] – https://www.ncbi.nlm.nih.gov/books/NBK53914/
[13] – https://www.tha.org/blog/build-a-model-of-recurring-revenue-with-ccm/
[14] – https://www.thoroughcare.net/blog/care-management-programs-revenue
[15] – https://www.medicaleconomics.com/view/analysis-of-ai-cognitive-threshold-identifies-cost-efficient-strategy-for-health-care-implementation
[16] – https://www.mountsinai.org/about/newsroom/2024/study-identifies-strategy-for-ai-cost-efficiency-in-health-care-settings
[17] – https://acarepro.abbott.com/articles/general-topics/role-of-ai-in-adherence/
Disclaimer
The information in this article is provided by HolistiCare for general informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. HolistiCare does not warrant or guarantee the accuracy, completeness, or usefulness of any information contained in this article. Reliance on any information provided here is solely at your own risk.
This content does not create a doctor-patient relationship. Clinical decisions should be made by qualified healthcare professionals using clinical judgment and all available patient information. If you have a medical concern, contact your healthcare provider promptly.
HolistiCare may reference biomarker roles, study examples, products, or tools. Mention of specific tests, biomarkers, therapies, or vendors is for illustrative purposes only and does not imply endorsement. HolistiCare is not responsible for the content of third party sites linked from this article, and inclusion of links does not represent an endorsement of those sites.
Use of HolistiCare software, services, or outputs should be in accordance with applicable laws, regulations, and clinical standards. Where required by law or regulation, clinical use of biomarker information should rely on validated laboratory results and regulatory approvals. HolistiCare disclaims all liability for any loss or damage that may arise from reliance on the information contained in this article.
If you are a patient, please consult your healthcare provider for advice tailored to your clinical situation. If you are a clinician considering HolistiCare for clinical use, contact our team for product specifications, regulatory status, and clinical validation documentation.


What do you think?
[…] in mind, clinics report that losing a patient costs between $100,000-$300,000 in lifetime value [21]. As patients visualize their biological aging slowing, they experience powerful “Aha!” […]