For the last decade, longevity medicine has been fighting a losing battle against its own infrastructure. You have likely felt it: the friction of trying to practice 21st-century precision medicine with 20th-century administrative tools.
Methodology (brief): This analysis synthesizes HolistiCare client pilot results, anonymized customer feedback, and public industry research (Jan–Dec 2025).
In our previous analysis, Why Legacy EHRs Fail Longevity Clinics at Scale, we diagnosed the core issue as “Operational Debt.” Static software creates friction that slows growth. But diagnosing the disease is the easy part. The real question—and the one dominating boardrooms in 2026—is: what is the cure?
We are witnessing a Great Migration. High-performing longevity clinics are no longer looking for marginally better EHRs. They are adopting a new infrastructure: the Clinical Intelligence Platform (CIP).
The “Data Dead End”
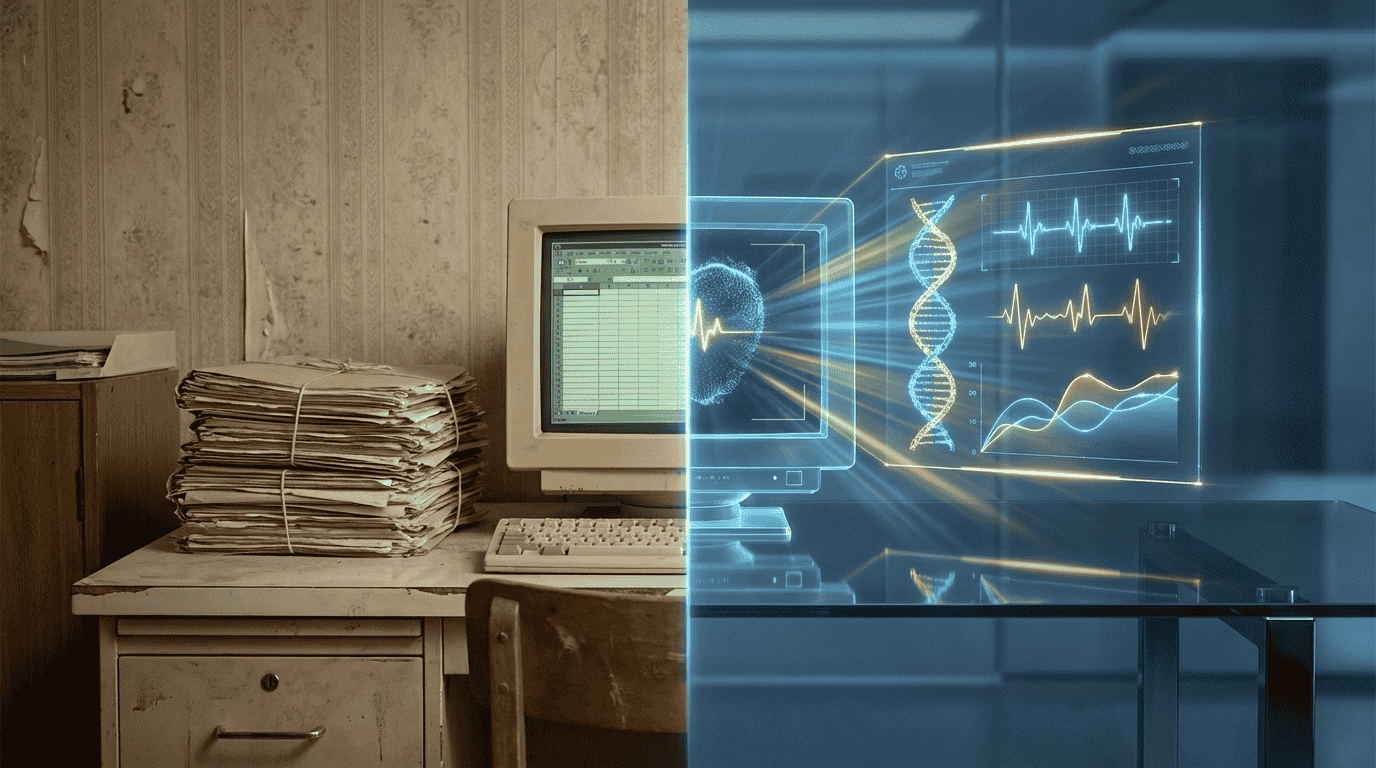
Why the shift now? Traditional EHRs were designed for acute care—episodic visits, billing codes, and compliance. They function as digital filing cabinets: good at storing a PDF, not at understanding trends. That design creates a “Data Dead End” for longevity clinics that rely on high-frequency longitudinal data.
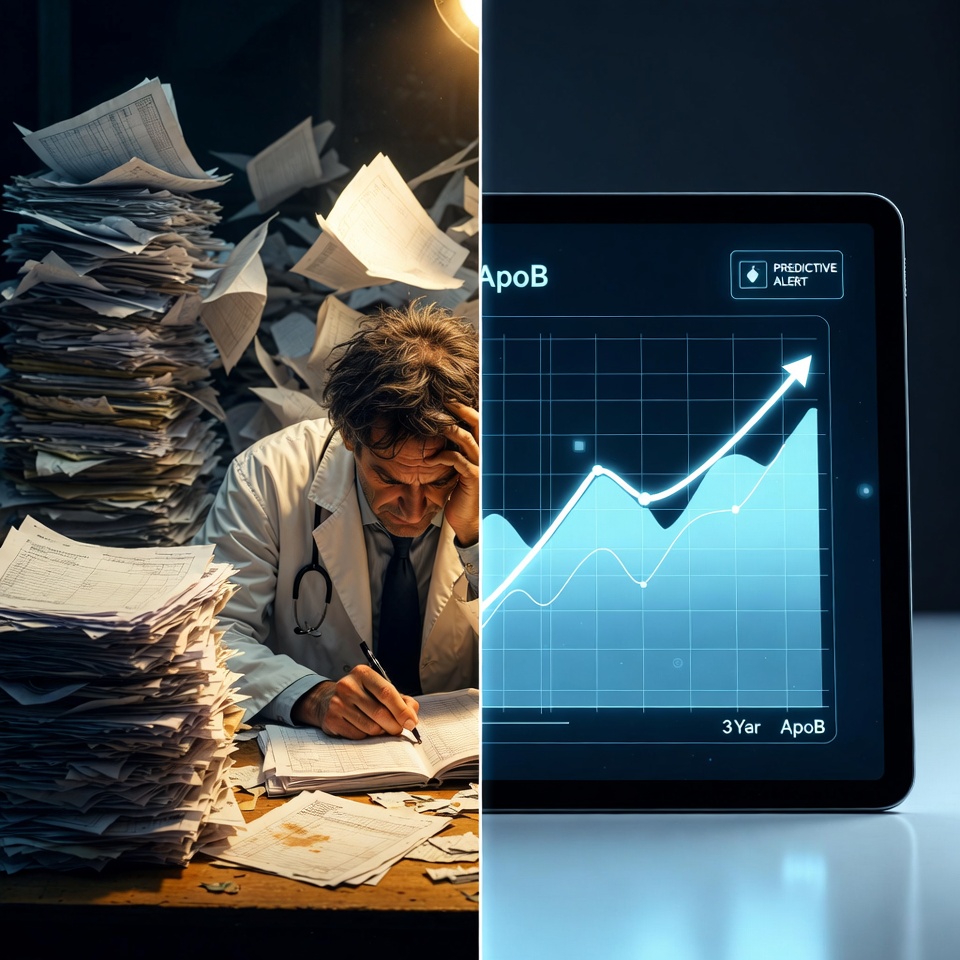
Data accumulation is not the problem—the inability to operationalize that data is. Research and time-motion studies show clinicians spend a large share of their shift interacting with EHRs and documentation tasks, which reduces time available for higher-value clinical work.
What is a Clinical Intelligence Platform (CIP)?
If an EHR is a digital filing cabinet, a CIP is a digital nervous system.
A CIP doesn’t just store data; it activates it—designed for longitudinal, high-frequency inputs and automated insight generation.
Three drivers of migration in 2026
Our synthesis of client pilots, customer feedback, and industry literature points to three urgent requirements:
1. The Need for “n=1” Analysis at Scale
Personalized longevity care demands longitudinal, individualized analysis. CIPs use AI to flag biomarker deviations and correlations automatically; that automation lets clinics scale patient panels without linear increases in physician hours. Client pilots report meaningful clinician time savings (see case studies).
2. Client expectations and wearables
Patients now bring wearable streams (Oura, Whoop, CGM) and consumer genetics. EHRs generally lack standardized ingestion and normalization pipelines for high-frequency device data; academic and industry reviews document material integration challenges. CIPs natively ingest, normalize, and visualize these streams alongside labs.
3. Automation of repetitive clinician work
The most expensive resource is clinician attention.
Traditional EHR workflows require manual curation and notes; CIPs automate intake, synthesis, and highlight actionable signals so clinicians start consults with presynthesized insights. Early evidence from pilot programs shows reduced admin time and faster onboarding.
The ROI of Intelligence vs. Administration
Switching systems is disruptive. But the cost of staying is real: lower clinician productivity, slower onboarding, and weaker retention.
Clinics that have migrated report operational benefits—improved retention, faster clinician onboarding, and lower per-patient admin time—though ROI will vary by implementation and patient mix. Where we cite specific performance figures, those are drawn from client pilots or published reports and are identified as such.
How to Start the Migration
You don’t need to rip out your entire infrastructure overnight. Most migrations start by layering intelligence in parallel to billing systems and gradually shifting operational responsibility as validation and workflows mature. Crucial first steps:
Define success metrics (physician minutes saved, retention, LTV uplift).
Run a short pilot with measurable KPIs.
Confirm data-security, interoperability, and regulatory requirements up front.
Request a demo of HolistiCare to see how a Clinical Intelligence Platform can turn your data into an operational advantage.
Disclaimer
The information in this article is for general informational purposes only and is not medical advice. Clinical decisions must be made by qualified healthcare professionals using full clinical context and validated lab results. Product performance claims are based on internal case studies and publicly available literature cited above; individual results may vary. HolistiCare recommends legal and compliance review before clinical deployment.