The economics of preventative health are compelling. For every dollar invested in disease prevention and health promotion, the economic return reaches 4.4 times through reduced healthcare costs and improved workforce productivity [1]. This financial reality, coupled with overwhelming patient demand, has pushed longevity medicine from specialized clinics into standard medical practice across the country.
How longevity medicine moved from "elite biohacking" to a standard request for the average patient in 2026
What was once considered exclusive “biohacking” has transformed into mainstream healthcare. By 2026, longevity technologies have firmly established themselves in hospitals, clinics, and wellness centers nationwide [1]. This shift reflects a fundamental change in how patients perceive healthcare—they’re no longer willing to wait until they’re sick to seek treatment.
The education system has responded accordingly. For the first time, Healthy Longevity Medicine has become mandatory curriculum for medical students. The Longevity Education Hub’s free, accredited curriculum has expanded into universities across six countries, with over 13,000 medical professionals enrolled in their courses as of October 2025 [1]. At universities like the State University of Makassar in Indonesia, medical students now receive 516 hours of longevity medicine education integrated throughout their training [1].
Jim Donnelly, CEO of Human Health, notes that the term “longevity” itself has evolved from sounding exclusive to becoming more inclusive. Many professionals now prefer the term “health optimization,” focusing on immediate benefits rather than distant promises [2]. This linguistic shift symbolizes the field’s democratization.
Market growth reflects this transformation. The wellness and longevity sector is projected to exceed $10 trillion globally by 2030 [2]. In the United States alone, approximately 800 longevity clinics are currently operating, with global investment more than doubling between 2021 and 2022 [2].
For medical directors and practice owners, this represents both challenge and opportunity. Your patients no longer compare their results to population averages—they want optimization, not normalization. They’re arriving with questions about biological age, not just cholesterol levels. As practitioners, you face a critical choice: adapt your practice to this new paradigm or watch patients migrate to clinics that have.
The New Standard Lab: Why basic metabolic panels are being replaced by biological age clocks (DunedinPACE) and multi-omic testing
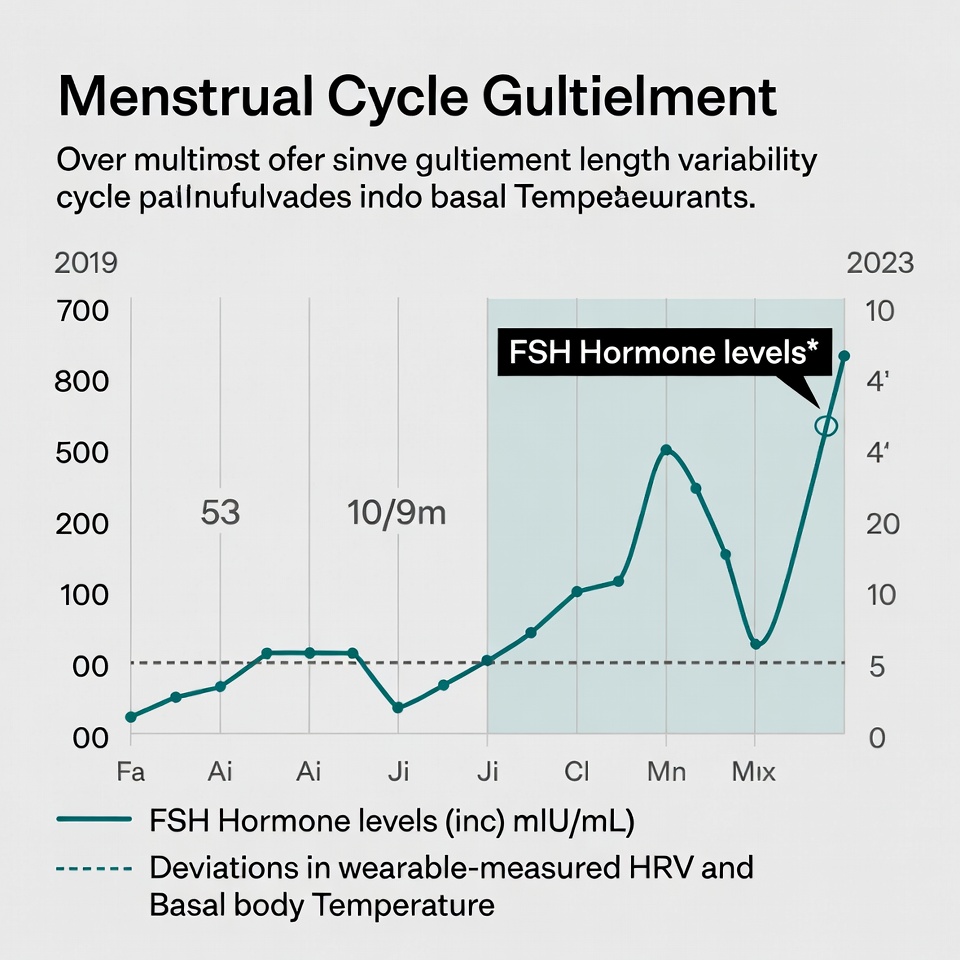
Biological age has emerged as the most important risk factor determining individual risk of morbidity and mortality [3]. Unlike chronological age, biological age can be modified—and patients know this. Forward-thinking clinics have responded by adopting new gold standards in assessment.
The DunedinPACE epigenetic clock stands at the forefront of this evolution. Unlike earlier measures that simply compared biological age to chronological age, DunedinPACE measures the pace of aging—how quickly or slowly a person is aging [4]. This crucial distinction makes it significantly more sensitive to interventions and lifestyle changes.
The data supporting DunedinPACE is compelling. Even slightly elevated aging rates (just above 1 biological year per chronological year) increase mortality risk by 56% and chronic disease risk by 54% over the following seven years [5]. Furthermore, it predicts cognitive decline, mild cognitive impairment, and dementia [4], making it invaluable for comprehensive patient assessment.
Multi-omic testing has similarly moved from luxury to necessity. Clinical-grade testing now examines:
Genomics: Identifying predispositions and personalized intervention targets
Proteomics: Measuring inflammatory markers and metabolic function
Metabolomics: Assessing cellular energy production and nutrient processing
Microbiome: Analyzing gut health and immune function
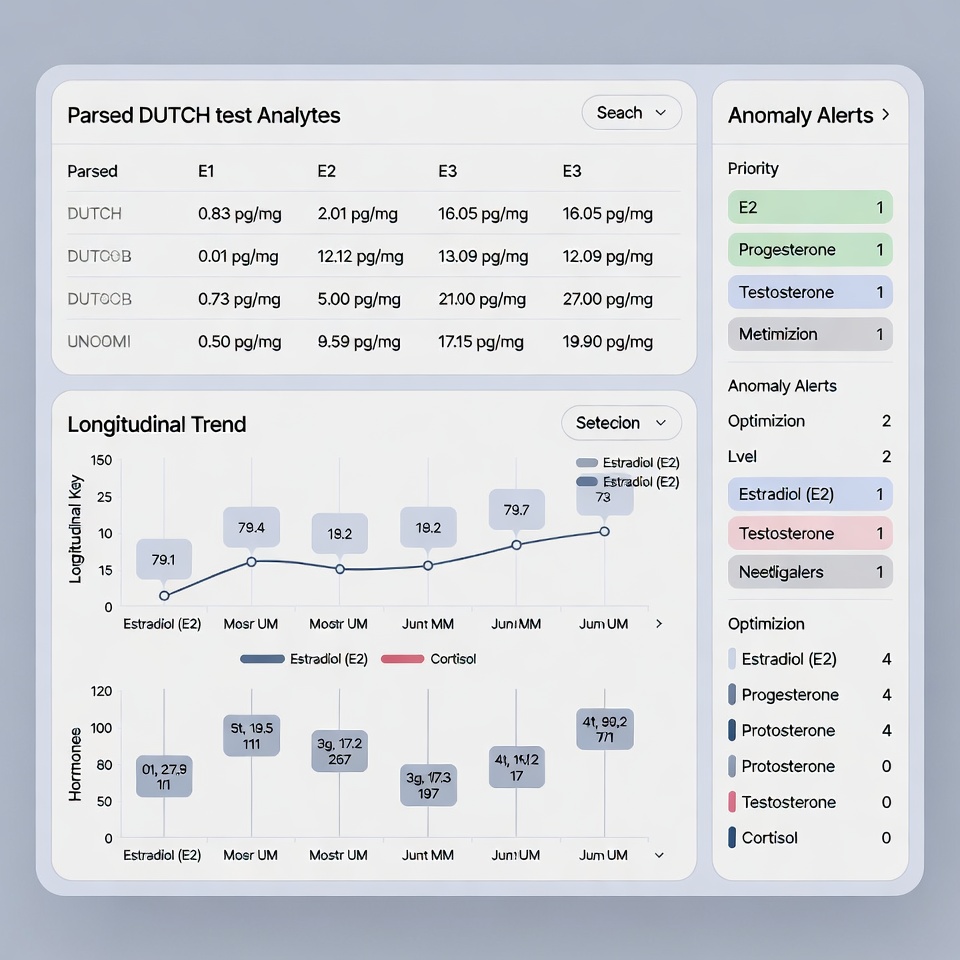
This data deluge presents a significant challenge for practitioners. With potentially 800+ biomarkers to interpret per patient, traditional analysis methods simply cannot scale. This is where clinical intelligence platforms like HolistiCare.io have become essential.
By automating the initial interpretation of complex datasets, these platforms save practitioners approximately 15 hours per week—time better spent on strategic patient care rather than data entry. Additionally, they ensure no critical patterns are missed in the overwhelming volume of information.
For practice owners, the integration of these technologies represents a competitive advantage. Practices offering biological age assessment and multi-omic testing report higher patient satisfaction and retention. However, the real differentiation comes from how this data is interpreted and applied.
The most successful clinics in 2026 have moved beyond simply collecting data to implementing systems that transform that data into actionable protocols. The practitioner’s role has evolved from data interpreter to strategic health architect, focusing on the interventions that will most meaningfully impact a patient’s longevity trajectory.
When implemented effectively, this approach yields measurable outcomes: reduced biological age, improved metabolic function, enhanced cognitive performance, and ultimately, increased healthspan. For medical directors, this translates to improved practice metrics, reduced practitioner burnout, and increased practice valuation.
The transition from reactive disease management to proactive longevity medicine requires investment—in education, technology, and workflow redesign. Nevertheless, the practices that have made this investment report not only improved clinical outcomes but also significant operational benefits, including streamlined protocols, reduced decision fatigue, and enhanced practice efficiency.
The Top 3 Clinical Trends
The clinical landscape of 2026 reveals a clear shift in how progressive medical practices approach health optimization. As clinicians embrace longevity medicine, three dominant trends have emerged that distinguish leading practices from those still caught in reactive care models.
Trend 1: Biological Age as the Primary KPI
For forward-thinking medical directors, traditional metrics like cholesterol levels and BMI have been supplanted by a more comprehensive indicator: biological age. Epigenetic clocks now serve as the gold standard for measuring patient progress, offering predictive insights into mortality and age-related disease risks with remarkable precision [6].
The shift toward biological age as a key performance indicator reflects an essential truth: chronological age fails to capture the actual physiological health of patients. Epigenetic clocks derived from DNA methylation patterns estimate biological age, effectively distinguishing it from chronological age and illuminating crucial questions in health optimization [3].
DunedinPACE has emerged as the industry-leading biological age assessment tool in 2026 practices. Unlike earlier clocks that simply compared biological to chronological age, DunedinPACE measures the pace of aging—offering superior sensitivity to interventions and lifestyle modifications [7]. Practice owners report that this distinction resonates powerfully with patients, who grasp that slowing their aging rate delivers more immediate benefits than merely appearing “younger than their years.”
The clinical value of these tools extends beyond mere age estimation. PhenoAge, another widely adopted clock, captures age-related shifts tied to cardiovascular disease, diabetes, cognitive decline, and all-cause mortality [3]. Moreover, it correlates with lifestyle factors including educational attainment, physical activity, income, blood pressure, BMI, dietary habits, and smoking status—creating a comprehensive snapshot of patient health [3].
Medical directors implementing biological age assessment report substantial benefits: precise evaluation of intervention effects, enhanced patient engagement, and most critically, the ability to demonstrate measurable improvement in a patient’s health trajectory. Practices utilizing epigenetic clocks as their primary KPI typically document intervention effectiveness within 3-6 months—a significant improvement over traditional metrics that might take years to show meaningful change.
Trend 2: The GLP-1 Metabolic Reset
The meteoric rise of GLP-1 receptor agonist prescriptions—a staggering 587% increase in the past five years [8]—has created both opportunities and challenges for clinicians. While these medications deliver impressive weight loss results, they come with a concerning side effect: lean body mass can account for 15-40% of total weight loss [8].
Leading clinics have responded by implementing comprehensive GLP-1 optimization protocols through clinical intelligence platforms like HolistiCare.io. These systems analyze hundreds of biomarkers to craft personalized metabolic reset programs that preserve muscle while enhancing fat loss.
The BELIEVE Phase 2b trial demonstrated the power of combination approaches, showing that bimagrumab (a drug targeting muscle loss) combined with semaglutide produced superior results: 92.8% of total weight loss came from fat mass compared to semaglutide alone (71.8%) [8]. This kind of nuanced protocol development—analyzing multiple interventions and their synergistic effects—is precisely where clinical intelligence shines.
Progressive medical directors recognize that muscle preservation requires a multifaceted approach. Beyond medication combinations, practices using HolistiCare report success with customized nutrition and exercise protocols:
High-protein diets that protect muscle mass during weight loss
Specific resistance training programs that stimulate muscle protein synthesis
Targeted supplementation based on individual biomarkers
Continuous monitoring using novel protein sensors that track lean muscle mass [8]
The data burden of this approach is substantial. Practitioners monitoring patients on GLP-1 therapies may track hundreds of biomarkers simultaneously—an impossible task without computational assistance. HolistiCare’s clinical intelligence layer saves practitioners an average of 15 hours weekly by automating the initial protocol draft, elevating the clinician from data entry clerk to chief strategist.
Trend 3: Personalized Microbiome & Gut-Brain Axis
Perhaps no area has evolved more rapidly than gut health optimization. The outdated approach of recommending generic probiotics has given way to sophisticated, AI-driven protocols that recognize the gut microbiome’s intricate relationship with overall health.
Contemporary research firmly establishes the bidirectional communication between the gut microbiome and central nervous system—the “microbiota-gut-brain axis” [9]. This connection provides essential cues to microglia, astrocytes, and oligodendrocytes, influencing immune regulation and disease progression [9]. Additionally, recent studies have revealed that the human gut microbiome is a major determinant of plasma metabolome, potentially exerting more influence than genetics [9].
Consequently, elite practices have transitioned from generic “take this probiotic” recommendations to comprehensive gut health programs driven by clinical-grade testing and AI analysis. These programs typically include:
First, in-depth microbiome analysis that identifies beneficial commensals, inflammatory pathobionts, and metabolic capabilities. Second, integration of this data with other biomarkers to create personalized intervention plans. Third, monitoring of gut-systemic connections, particularly focused on immune regulation, neurotransmitter production, and inflammatory markers.
Throughout 2025, clinical trials demonstrated that personalized microbiome interventions significantly improved gut diversity metrics, with patients at post-intervention showing higher gut microbiota diversity and richness compared to baseline [10]. Intriguingly, studies identified specific bacterial genera that exhibited significant changes following personalized dietary interventions, including increases in beneficial organisms with cholesterol-reducing properties [10].
The microbiome serves as “an excellent checkpoint for biological deviations, reflecting the body’s overall state” [11]. Forward-thinking practice owners have recognized this, integrating microbiome data with neurobiology, immunology, and systemic biology to map and modulate entire body systems [11].
These three clinical trends converge in the practices of 2026’s most successful clinicians. By measuring progress through biological age, optimizing GLP-1 therapies for ideal body composition, and implementing personalized microbiome protocols, leading practitioners have redefined the standard of care.
For medical directors and practice owners, the challenge isn’t whether to adopt these approaches—it’s how quickly they can implement the clinical intelligence layer necessary to manage the resulting complexity. With patients generating 800+ biomarkers through modern testing panels, the practices that thrive are those that have systematized data management through platforms like HolistiCare.io, freeing clinicians to focus on strategic decision-making rather than drowning in data.
The Role of Clinical Intelligence (CI)
In today’s data-saturated clinical environment, the difference between thriving and merely surviving practices hinges on a crucial element: Clinical Intelligence (CI). This emerging layer of technological infrastructure stands as the essential bridge between raw data and actionable insights for longevity-focused clinicians.
Automating the Data Deluge
The modern longevity practice faces an unprecedented challenge: managing the sheer volume of patient data. HolistiCare’s platform automatically processes over 800 biomarkers from blood, genetics, microbiome, and lifestyle data [4], transforming what was once a manual analytical burden into a streamlined clinical workflow.
Before CI platforms, clinicians spent substantial time manually normalizing units, reconciling reference ranges, and hunting for clinically relevant trends across disjointed vendor reports [5]. This fragmentation created critical problems: slower decision-making from cross-referencing PDFs, inconsistent data across providers, and reduced capacity for high-value patient care [5].
HolistiCare acts as a central intelligence layer by ingesting multi-vendor data, standardizing it into a canonical model, and applying a transparent interpretation layer trained in clinical and longevity medicine [5]. The system eliminates manual data entry through direct integration with lab information systems and electronic health records [4], effectively transforming how practitioners approach patient data:
Auto-Normalization: The platform automatically handles unit conversions (e.g., mmol/L to mg/dL) and maps vendor-specific reference ranges to age/sex-specific intervals [5]
Pattern Recognition: Instead of presenting clinicians with isolated abnormal results, the system identifies clinically meaningful patterns and ranks them by probable impact [5]
Comprehensive Integration: The platform standardizes biomarker data from diverse sources into unified reports highlighting clinically relevant patterns [4]
Essentially, this automation shifts the practitioner’s focus from data management to strategic interpretation and care planning.
The 15-Hour ROI
Practitioner burnout has reached crisis levels, with documentation burden identified as a major contributor [12]. HolistiCare addresses this directly by dramatically accelerating the creation of patient care plans through automated biomarker analysis, reducing the time needed to produce first drafts of clinical reports by 56%—cutting average preparation time from 180 hours to just 80 hours [4].
After analyzing biomarker data, the AI generates draft treatment plans based on established protocols and peer-reviewed research, including supplement recommendations, dietary modifications, and lifestyle interventions specifically tailored to address identified biomarker imbalances [4]. The system ranks interventions by potential impact and provides scientific rationales for each recommendation [4].
The ROI extends beyond time savings. Recent research shows that implementing ambient AI technology correlates with clinically meaningful reduction in burnout scores and decreased work outside office hours by 30 minutes per day per provider [13]. Practitioners using such technology report improved clinical experiences with comments like “improves joy in practice” and increased “contact with patients and families” [12].
Previously, practitioners produced plans addressing single health pillars; now AI combines biomarkers, genetics, lifestyle, and behavior into clinician-reviewable holistic plans spanning diet, exercise, sleep, and mental health domains [2].
Transparency and Trust
For AI to be embraced in clinical settings, explainability is paramount. HolistiCare prioritizes this through “Explainable AI” (XAI) methods that provide both global explanations (showing how features generally influence predictions) and local explanations (interpreting single predictions for specific patients) [14].
For every automated inference, the platform displays a short, clinician-readable rationale: which values drove the inference, relevant thresholds, and linked references to guidelines or primary literature [5]. This approach builds trust by making the “black box” transparent.
The ENABL Age study demonstrates the power of explainable AI in clinical settings. For individual patients, the system identifies specific features that increase or decrease biological age, such as “sex-hormone-binding globulin” or “never having past tobacco smoking,” providing granular insights that clinicians can use for targeted interventions [15].
Ultimately, clinical intelligence succeeds when it supports rather than replaces clinical expertise. HolistiCare’s platform ensures clinicians retain control and can intervene at any stage, dictating workflow priorities through an intuitive review and editor interface [2]. The AI-generated recommendations serve as well-researched starting points that doctors can modify based on their professional judgment and patient-specific needs [4].
For medical directors charting their 2026 strategy, the message is clear: the future belongs to clinician-led, AI-enhanced care that transforms practitioners from data managers to strategic health architects.
Operationalizing Longevity for Q1 2026
As we approach 2026, the longevity medicine revolution stands at a critical inflection point. Certainly, what began as elite biohacking has transformed into standard care demanded by patients across all demographics. Your patients no longer accept “normal” lab values—they expect optimization and personalization based on their unique biological profile.
This paradigm shift presents both challenge and opportunity for forward-thinking medical directors. The practices thriving today have successfully transitioned from reactive disease management to proactive longevity optimization through three key clinical approaches: measuring biological age as the primary KPI, implementing comprehensive GLP-1 protocols that preserve muscle mass, and developing personalized microbiome interventions that address the gut-brain axis.
Nevertheless, the complexity of managing 800+ biomarkers per patient creates an unsustainable burden without proper technological support. Clinical Intelligence platforms like HolistiCare.io have therefore become essential practice infrastructure, saving practitioners approximately 15 hours weekly by automating initial protocol drafts while preserving clinical judgment.
Your role as a practitioner has fundamentally evolved from data entry clerk to chief health strategist. Those embracing this evolution report not only improved clinical outcomes but also significant practice benefits: higher patient retention, reduced burnout, and enhanced practice valuation.
The economics tell a compelling story—for every dollar invested in preventative health approaches, the return reaches 4.4 times through reduced costs and improved outcomes. This financial reality, coupled with overwhelming patient demand, makes longevity medicine not merely a specialization but a fundamental practice evolution.
The choice facing medical directors today is straightforward: adapt your practice to this new paradigm or watch patients migrate to clinics that have. Though implementation requires investment in education, technology, and workflow redesign, practices making this transition report significantly improved efficiency, practitioner satisfaction, and patient outcomes.
Ultimately, the future belongs to clinician-led, AI-enhanced care that transforms healthcare from sickness management to proactive optimization. Your patients are already demanding this approach—the question remains whether your practice will lead this transformation or follow behind.
Key Takeaways
Longevity medicine has evolved from elite biohacking to mainstream healthcare, with patients now demanding optimization over normalization and biological age assessment becoming the new standard of care.
• Biological age is the new primary metric: Epigenetic clocks like DunedinPACE now measure aging pace, providing actionable insights within 3-6 months versus years with traditional markers.
• GLP-1 therapy requires comprehensive protocols: Leading clinics use AI platforms to preserve muscle mass during weight loss, as 15-40% of GLP-1 weight loss can be lean muscle.
• Clinical Intelligence platforms save 15 hours weekly: Automated biomarker analysis of 800+ data points transforms practitioners from data managers to strategic health architects.
• Personalized microbiome protocols replace generic probiotics: AI-driven gut health interventions address the gut-brain axis using clinical-grade testing and targeted interventions.
• ROI is compelling at 4.4x return: Every dollar invested in preventative longevity medicine yields $4.40 in reduced healthcare costs and improved productivity.
The practices thriving in 2026 have embraced this evolution, reporting higher patient retention, reduced practitioner burnout, and enhanced practice valuation through systematic implementation of longevity-focused protocols and clinical intelligence systems.
FAQs
Q1. What is the primary metric used in longevity medicine in 2026? Biological age has become the primary metric in longevity medicine. Clinics are using epigenetic clocks like DunedinPACE to measure the pace of aging, providing more actionable insights than traditional health markers.
Q2. How are clinics managing patients on GLP-1 therapies for weight loss? Leading clinics are using clinical intelligence platforms to develop comprehensive protocols for patients on GLP-1 therapies. These protocols aim to preserve muscle mass during weight loss, as 15-40% of weight loss from GLP-1 therapies can come from lean muscle.
Q3. What role does artificial intelligence play in longevity medicine practices? AI, particularly through Clinical Intelligence (CI) platforms, plays a crucial role in synthesizing and analyzing large amounts of patient data. These platforms can process over 800 biomarkers, saving practitioners an average of 15 hours per week and allowing them to focus on strategic patient care.
Q4. How has the approach to gut health changed in longevity medicine? The approach has moved beyond generic probiotic recommendations to personalized, AI-driven gut health protocols. These protocols are based on clinical-grade microbiome testing and take into account the gut-brain axis, aiming to optimize overall health through targeted interventions.
Q5. What is the economic benefit of investing in longevity medicine? The return on investment for preventative longevity medicine is compelling, with every dollar invested yielding a 4.4 times return through reduced healthcare costs and improved productivity. This economic reality, combined with patient demand, is driving the widespread adoption of longevity medicine practices.
References
[1] – https://longevity.technology/news/longevity-medicine-enters-med-school/
[2] – https://holisticare.io/
[3] – https://pmc.ncbi.nlm.nih.gov/articles/PMC12539533/
[4] – https://holisticare.io/blog/biomarker-analysis/
[5] – https://holisticare.io/features/clinical-data-analysis-software/
[6] – https://www.sciencedirect.com/science/article/pii/S1471491425002576
[7] – https://www.thelancet.com/journals/lanhl/article/PIIS2666-7568(22)00114-3/fulltext
[8] – https://diabetes.org/newsroom/press-releases/new-glp-1-therapies-enhance-quality-weight-loss-improving-muscle-0
[9] – https://www.nature.com/articles/s41392-024-01743-1
[10] – https://www.mdpi.com/2072-6643/17/7/1260
[11] – https://www.nutraingredients.com/Article/2025/01/15/ai-personalized-microbiome-modulation-for-longevity/
[12] – https://www.medpagetoday.com/practicemanagement/informationtechnology/117111
[13] – https://www.uwhealth.org/news/research-shows-ambient-ai-improves-healthcare-practitioner-well-being
[14] – https://www.mdpi.com/2076-3417/15/15/8449
[15] – https://www.thelancet.com/journals/lanhl/article/PIIS2666-7568(23)00189-7/fulltext
Disclaimer
The information in this article is provided by HolistiCare for general informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. HolistiCare does not warrant or guarantee the accuracy, completeness, or usefulness of any information contained in this article. Reliance on any information provided here is solely at your own risk.
This content does not create a doctor-patient relationship. Clinical decisions should be made by qualified healthcare professionals using clinical judgment and all available patient information. If you have a medical concern, contact your healthcare provider promptly.
HolistiCare may reference biomarker roles, study examples, products, or tools. Mention of specific tests, biomarkers, therapies, or vendors is for illustrative purposes only and does not imply endorsement. HolistiCare is not responsible for the content of third party sites linked from this article, and inclusion of links does not represent an endorsement of those sites.
Use of HolistiCare software, services, or outputs should be in accordance with applicable laws, regulations, and clinical standards. Where required by law or regulation, clinical use of biomarker information should rely on validated laboratory results and regulatory approvals. HolistiCare disclaims all liability for any loss or damage that may arise from reliance on the information contained in this article.
If you are a patient, please consult your healthcare provider for advice tailored to your clinical situation. If you are a clinician considering HolistiCare for clinical use, contact our team for product specifications, regulatory status, and clinical validation documentation.


What do you think?
[…] This automation shifts the practitioner’s focus from data management to strategic interpretation and care planning, reducing the time needed to produce clinical reports by 56%—cutting average preparation time from 180 hours to just 80 hours [17]. […]
[…] Biological Age Tests Measure Aging 12 Longevity Trends Doctors Are Watching in 2026 Biomarkers of Aging Consortium Longevity Science Crosses Clinical Threshold Longevity Medicine 2026 Strategy […]
[…] over lifespan, moving away from generalized wellness toward individualized protocols based on epigenetic clocks like […]