For many longevity clinic owners, the choice of EHR was pragmatic: it fit the early budget, a lead practitioner knew it already, or it felt like the least bad option among platforms designed primarily for primary care and insurance billing.
For a single location with a small patient panel, “good enough” often works. Inefficiencies are manageable; manual workarounds are annoying, but survivable.
As a clinic scales—moving from one location to several, or from hundreds of members to thousands—the relationship with your software changes. What was once a minor daily nuisance becomes a structural anchor that drags down operations.
For many established longevity and functional medicine organisations, the realization is blunt: the EHR that got you here is unlikely to be the infrastructure that gets you there.
Methodology: This article reflects HolistiCare’s experience working with longevity clinics, anonymized client feedback, and a review of publicly available industry literature.
This piece doesn’t focus on bugs or vendor failures. It examines a deeper structural mismatch between legacy healthcare software architecture and the operational reality of longitudinal, data-driven care.
The “Acute Care” Architecture vs. The Longevity Model
Legacy EHRs were architected for acute, episodic, insurance-based care. In that model, interactions are discrete: a visit occurs, a diagnosis is coded, a claim is submitted, and the record becomes dormant until the next encounter. Software is optimized for brevity, throughput, and billing workflows.
Longevity medicine operates on different premises: care is longitudinal, data is continuous, and value accumulates over years rather than single visits. Clinics ingest genomics, microbiome panels, CGM streams, and wearable biometrics; they manage multi-phase protocols involving supplements, peptides, and lifestyle interventions.
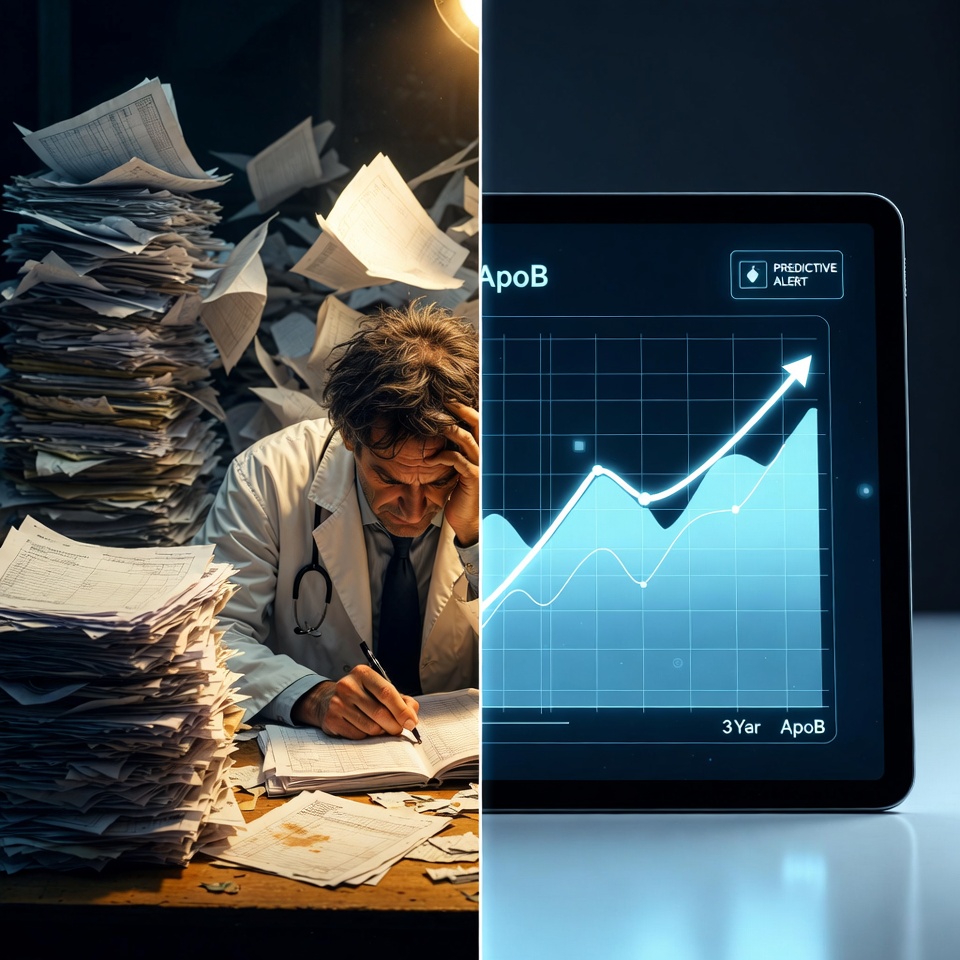
Forcing a longevity model into an acute-care architecture produces operational friction: the system assumes closure; longevity care assumes continuity. The system organizes by encounter date; longevity care needs trend lines. Over time, that friction compounds into operational debt.
The Three Phases of Operational Failure
Operational debt behaves like financial interest: early on you pay it with human effort, later the payments become unsustainable.
1. Data Fragmentation (The “Alt-Tab” Tax)
Legacy EHRs often cannot natively ingest, normalize, or visualize diverse continuous data streams. Clinical teams end up juggling multiple windows and tools—the EHR, lab PDFs, spreadsheets, membership platforms, and device portals. Each context switch erodes efficiency and increases the risk of missed correlations between interventions and biomarker responses.
2. The “Hero” Dependency
Workflows survive because one or two people know the workarounds. That institutional knowledge becomes a single point of failure. When a “hero” leaves, the process fractures. Scaling to new locations reveals whether your operations are systematized or person-dependent.
3. The Analytics Black Box
C-suite leaders need answers to operational questions—protocol performance, cost per member, capacity utilization, provider variance in retention. Legacy EHRs can store data, but extracting cross-patient, real-time intelligence often requires manual reporting or external tooling. The practical consequence is slower decisions and reliance on anecdote rather than operational intelligence.
The Strategic Risks of Status Quo
Many clinics delay migration because of the perceived disruption. That calculation made sense in earlier market conditions, but in 2026 the balance of risk has shifted.
A. The Growth Ceiling
Systems that resist standardization cap expansion; adding locations should not require linearly more administrative headcount.
B. The Competitive Risk
New entrants launch with intelligence-first stacks that automate engagement, visualize progress for members (which supports retention), and enable rapid protocol iteration based on aggregate data.
C. The Talent Risk
Clinicians want to practice medicine, not data entry. Administrative burden is a primary driver of burnout and turnover.
Why Customization Is a Trap
Many clinics try to retrofit legacy EHRs with custom integrations, third-party CRMs, or automation tooling. These “Franken-stacks” increase fragility and maintenance overhead. Customization can extend life briefly, but it rarely changes underlying architectural limits and makes future migration harder.
Read more on why clinics are switching to Clinical Intelligence Platforms in 2026.
The Shift: From Electronic Records to Clinical Intelligence
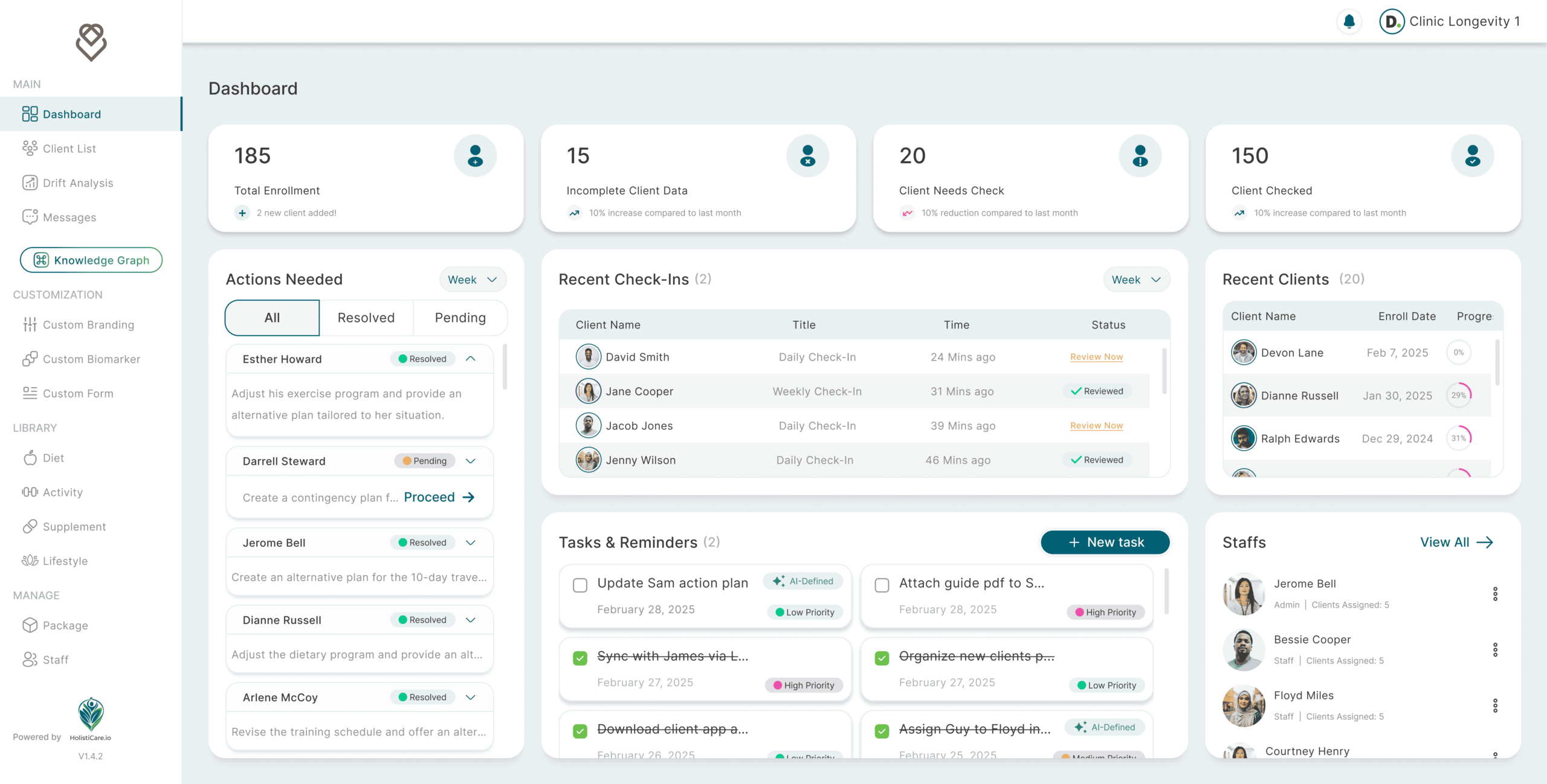
The solution is not a marginally better filing cabinet. It is a different category: Clinical Intelligence Platforms (CIP). A CIP is designed for:
Interoperability — ingesting data from labs, devices, and apps into a unified record;
Longitudinal visualization — plotting trends over time rather than isolated snapshots;
Operational transparency — dashboards that surface capacity, retention, and protocol performance in near real-time.
Adoption is often incremental: keep the EHR for billing and compliance while layering an intelligence system that handles care orchestration and decision support. Importantly, any migration must be planned with security, privacy, and regulatory alignment in mind.
Conclusion: The Cost of Waiting
Operational debt compounds with every new patient, data stream, and protocol. The largest cost is not the technical effort to move data; it is the opportunity cost of constrained growth and delayed decisions.
If your team spends more time reconciling spreadsheets than acting on insight, it is time to reassess the foundation beneath your growth.
Disclaimer
The information in this article is provided by HolistiCare for general informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. HolistiCare does not warrant or guarantee the accuracy, completeness, or usefulness of any information contained in this article. Reliance on any information provided here is solely at your own risk.
This content does not create a doctor-patient relationship. Clinical decisions should be made by qualified healthcare professionals using clinical judgment and all available patient information. If you have a medical concern, contact your healthcare provider promptly.
HolistiCare may reference biomarker roles, study examples, products, or tools. Mention of specific tests, biomarkers, therapies, or vendors is for illustrative purposes only and does not imply endorsement. HolistiCare is not responsible for the content of third party sites linked from this article, and inclusion of links does not represent an endorsement of those sites.
Use of HolistiCare software, services, or outputs should be in accordance with applicable laws, regulations, and clinical standards. Where required by law or regulation, clinical use of biomarker information should rely on validated laboratory results and regulatory approvals. HolistiCare disclaims all liability for any loss or damage that may arise from reliance on the information contained in this article.
If you are a patient, please consult your healthcare provider for advice tailored to your clinical situation. If you are a clinician considering HolistiCare for clinical use, contact our team for product specifications, regulatory status, and clinical validation documentation.
All claims and statistics are based on cited studies and industry reports as of 2026. Individual results may vary; consult healthcare professionals for personalized advice. HolistiCare features are designed to support evidence-based holistic care.