Did you know that 15-40% of weight loss from GLP-1 therapies comes from lean muscle mass, not fat?
While GLP-1 receptor agonists like semaglutide and dual GLP-1/GIP receptor agonists such as tirzepatide deliver impressive weight loss results—with semaglutide achieving 15% mean weight loss over 68 weeks and tirzepatide producing 15-21% in 72 weeks —this success comes with a hidden cost. In fact, the popularity of these medications has skyrocketed, with the number of Americans using incretin-based therapies increasing by 587% in just the last five years .
However, this rapid adoption creates a serious clinical concern you need to address: the Sarcopenia Emergency. When patients lose substantial muscle mass during weight loss treatment, they face increased risks of frailty and metabolic instability—essentially creating a longevity disaster that undermines the very health benefits they sought.
The solution isn’t abandoning these effective medications but rather implementing a targeted GLP-1 Muscle Preservation Protocol. Research shows that strategies including protein intake above 1.2 g/kg/day combined with structured resistance training can help preserve crucial lean mass . Furthermore, precision nutrition approaches featuring smaller, nutrient-dense meals rich in high-quality protein are becoming essential components of responsible GLP-1 therapy management .
This article will guide you through building a comprehensive clinical intelligence system to protect your patients’ muscle mass while maximizing the benefits of GLP-1 therapies—transforming your practice from simple “weight loss provider” to “strategic health architect.”
Implementing a Clinical Intelligence Layer
The sheer complexity of tracking muscle preservation during GLP-1 therapy requires a robust infrastructure. At the present time, most clinics struggle with what we call the “Data Chaos Problem” – a foundational issue that must be solved before implementing any effective GLP-1 Muscle Preservation Protocol.
Solving Data Chaos
Modern healthcare generates extraordinary volumes of physiological data, with monitoring systems alone producing over 1440 data points hourly that exceed human cognitive processing limits [1]. Consequently, healthcare leaders are now exploring intelligence layers built on top of EHRs—systems that can predict early outcomes through artificial intelligence and unlock the value of critical data buried inside [2].
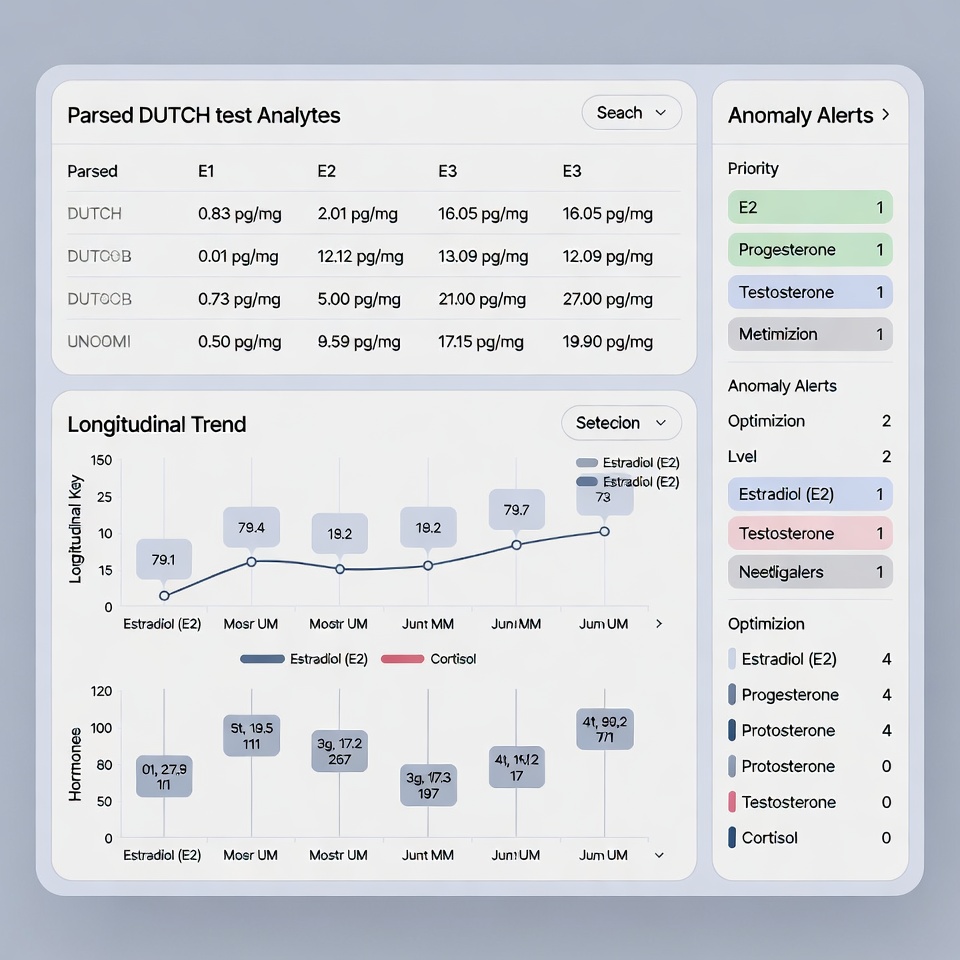
The challenge is that approximately 70% of patient data resides outside EMRs in disparate systems [3]. This creates what we call the “PDF Graveyard” – where crucial biomarker reports sit unanalyzed in disconnected formats. Clinical intelligence solves this by connecting data across various datasets—electronic health records, lab results, imaging, genomics—to present actionable insights specifically for muscle preservation [2].
The Clinical Intelligence (CI) layer auto-normalizes measurements between reagent lots, notably decreasing variability in longitudinal data [4]. This normalization is essential for tracking subtle changes in muscle biomarkers over time.
Standardization
Traditional clinical data collection has primarily relied on manual record abstraction and data entry [5]. Given these points, clinics implementing GLP-1 protocols face a significant bottleneck: recording just one data point every 1.11 minutes.
Electronic data processing and automated ingestion models offer superior alternatives. Studies show electronic processing yields more comprehensive patient datasets than manual methods [5]. Modern Clinical Data Ingestion (CDI) improves quality by automating data transfer specifications and identifying data quality risk predictions [6].
Coupled with advanced algorithms that sift through noise to uncover trends and patterns [7], this automation translates raw data into visual dashboards and timely alerts that enable healthcare professionals to make informed decisions about patients experiencing glp-1 muscle loss or tirzepatide muscle loss.
Phase 1: Configuring the 'Muscle Defense' Dashboard
Once your clinical intelligence infrastructure is established, configuring a proper ‘Muscle Defense’ dashboard becomes the cornerstone of an effective GLP-1 Muscle Preservation Protocol. This dashboard acts as your early warning system against dangerous muscle catabolism.
Key Biomarker Selection
Protein turnover—the continuous process of protein synthesis and degradation—is fundamental to muscle preservation. At a steady state, this process maintains protein homeostasis, yet disruptions can lead to pathological states [8]. For patients on GLP-1 therapy, monitoring this balance becomes critical.
Creatinine and Cystatin C form the foundation of your monitoring protocol. Serum creatinine reflects both kidney function and muscle mass, being significantly affected by factors including age, body size, and nutritional status [9]. Conversely, Cystatin C provides a more precise measure of kidney function since it remains unrelated to muscle mass [9].
The ratio between these markers—known as CCR (serum creatinine/serum cystatin C)×100—serves as a validated “sarcopenia index” with excellent correlation to muscle mass measurements [10]. Studies demonstrate CCR has significant correlations with handgrip strength (Fisher’s Z = 0.39) and gait speed (Fisher’s Z = 0.25) [10].
Albumin similarly offers critical insights, as declining levels strongly correlate with excessive skeletal muscle loss [11]. Research shows patients with excessive muscle loss (>10%/50 days) demonstrate significantly larger decreases in albumin compared to those maintaining muscle mass (-13.01% vs. -6.90%) [11].
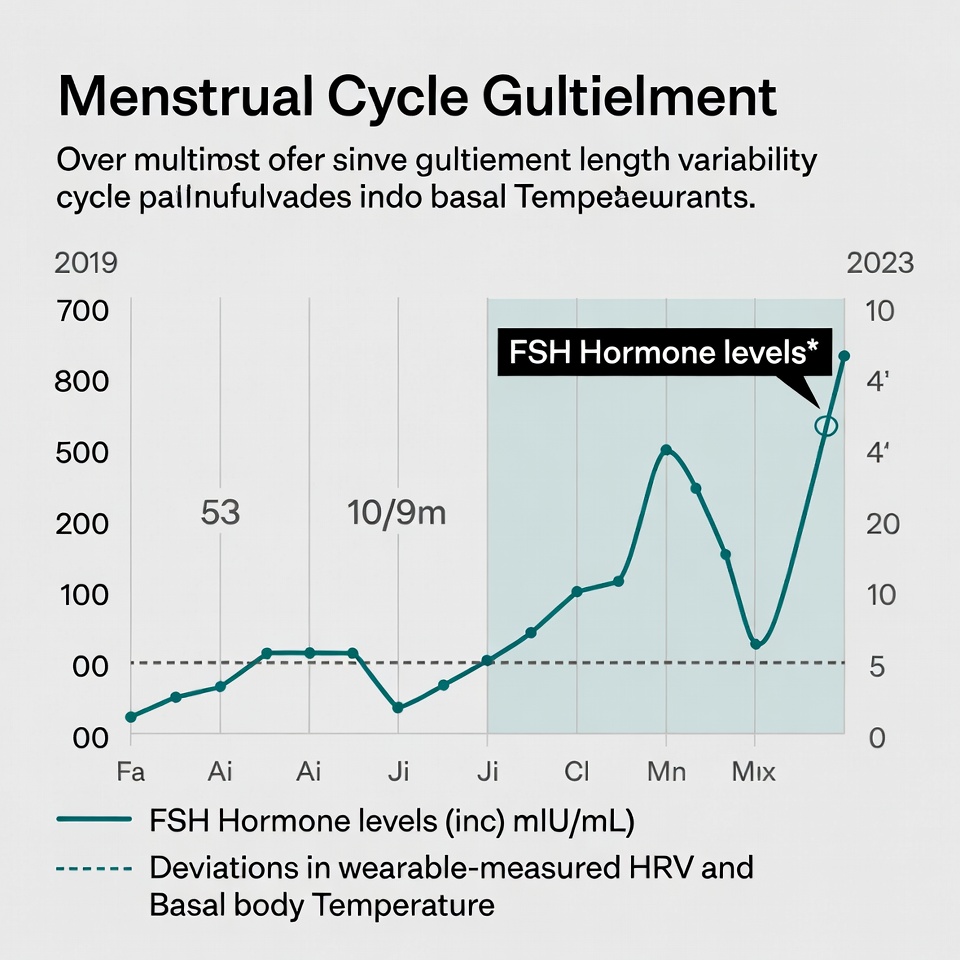
Neural Network Early Detection
Traditional DEXA scans, though valuable, only identify muscle loss after significant catabolism has occurred. Additionally, standard approaches distill rich imaging data into just a handful of metrics, discarding potentially valuable information about fat and muscle distribution [12].
HolistiCare’s neural networks transform this paradigm through advanced pattern recognition. Similar approaches using recurrent neural networks have already demonstrated superior accuracy in predicting 10-year mortality based on body composition data [12].
These models dramatically outperform single-record assessments—combined AUROC (Area Under Receiver Operating Characteristic) of 0.79 versus 0.71—demonstrating the power of longitudinal multivariate analysis [12]. Applied to GLP-1 monitoring, this means identifying subtle catabolism signals weeks before conventional methods.
Recent research confirms this approach’s validity, with AI models achieving remarkable accuracy (AUC between 0.92-0.94) in predicting muscle mass loss using just six anthropometric variables [13]. Even simpler models restricted to lower limb variables maintain impressive accuracy (AUC 0.88–0.90) [13].
Phase 2: Automated Nutritional & Resistance Interventions
After establishing your monitoring infrastructure, the next critical phase of the GLP-1 Muscle Preservation Protocol focuses on automated interventions that dynamically adapt to patient data.
Adaptive Protein Targets
Adequate protein intake remains paramount for fat-free mass preservation during GLP-1 therapy. Research confirms protein intake is positively associated with fat-free mass preservation, with studies showing 5.1% higher FFM in men and 7.7% higher FFM in women per 0.5-g/kg/day increment in protein intake [14]. Accordingly, for cancer patients and those experiencing rapid weight loss, protein supplementation consistently above 1.2 g/kg/day helps avoid significant muscle mass loss [15].
AI-powered nutrition platforms now enable dynamic protein target adjustments based on individual physiological variables. These systems incorporate deep learning components that generate personalized meal plans considering dietary preferences and lifestyle factors [16]. Additionally, such platforms offer:
Workflow Orchestration
Workflow optimization through automation addresses a critical efficiency gap in GLP-1 protocol management. Traditional clinical data collection primarily relies on manual record abstraction and time-consuming data entry [17]. Subsequently, implementing automated protocol drafting systems offers substantial time savings.
This automation transforms raw data into visual dashboards with timely alerts, enabling healthcare professionals to make informed decisions about patients experiencing GLP-1 muscle loss. Hence, the workflow analysis aims to optimize healthcare processes by reducing waste and improving clinical communication [17]. The result: a 56% reduction in report preparation time, effectively reclaiming 15 hours per week that clinicians can reallocate to direct patient care.
Phase 3: The Exit Strategy & Long-Term Retention
The final phase of any effective GLP-1 Muscle Preservation Protocol must address what happens after medication discontinuation. Clinical studies show patients typically regain two-thirds of lost weight within one year after stopping GLP-1 therapy [18].
Safe Transitioning
Generally, abrupt discontinuation creates metabolic instability as ghrelin levels surge, increasing hunger and food preoccupation [19]. Instead, gradual tapering over 9+ weeks allows patients to maintain or even continue losing weight [19]. Throughout this transition, your clinical intelligence dashboard should monitor protein turnover markers closely to prevent accelerated muscle catabolism.
Biological Age Tracking
Equally important is implementing biological age tracking via DunedinPACE—a validated epigenetic biomarker that uniquely measures the pace of aging rather than just biological age [20]. Unlike other aging clocks, DunedinPACE:
-
Captures how fast a person is aging at present [20]
-
Was validated across 65+ cohorts in 17+ countries [20]
-
Shows superior sensitivity to interventions [20]
With this purpose in mind, clinics report that losing a patient costs between $100,000-$300,000 in lifetime value [21]. As patients visualize their biological aging slowing, they experience powerful “Aha!” moments that drive long-term retention [21], effectively maintaining the economic foundation of your practice.
Conclusion
GLP-1 therapies undoubtedly deliver impressive weight loss results, though the hidden cost of losing 15-40% of lean muscle mass creates a significant clinical challenge. Therefore, implementing a comprehensive Muscle Preservation Protocol becomes essential for responsible patient care. Your practice must evolve beyond simple weight management to address this Sarcopenia Emergency effectively.
The three-phase approach outlined above provides you with a roadmap for transforming weight loss treatment. First, establishing the Clinical Intelligence infrastructure eliminates data chaos and enables meaningful biomarker tracking. Subsequently, configuring the Muscle Defense Dashboard with critical biomarkers like Creatinine, SHBG, Albumin, and Cystatin C allows early detection of muscle catabolism. Neural network analysis then identifies concerning patterns weeks before traditional methods would reveal them.
Automated nutritional and resistance interventions constitute the second vital phase of this protocol. AI-powered systems dynamically adjust protein targets based on individual patient data while workflow orchestration reclaims valuable clinical time. This efficiency gain – 15 hours weekly from a 56% reduction in report preparation time – allows you to focus more on direct patient care.
Perhaps most importantly, the Exit Strategy ensures patients transition safely off medications without experiencing metabolic crash. DunedinPACE tracking serves as your “speedometer for aging,” creating those powerful “Aha!” moments that secure long-term patient retention and maximize lifetime value.
Altogether, this muscle-centric approach addresses the fundamental flaw in conventional GLP-1 protocols. Patients receive the weight loss benefits they seek while preserving crucial muscle mass for long-term health. Your practice, meanwhile, positions itself as a strategic health architect rather than merely a weight loss provider. This comprehensive system not only protects patients from unnecessary frailty risks but also establishes your clinic as a leader in responsible metabolic health management.
Key Takeaways
GLP-1 therapies like semaglutide and tirzepatide create a hidden crisis: 15-40% of weight loss comes from muscle mass, not fat, leading to increased frailty risks and metabolic instability that undermines long-term health goals.
• Implement Clinical Intelligence Infrastructure: Auto-normalize 800+ biomarkers to eliminate “PDF graveyards” and reduce manual data entry from 1.11 minutes per point to automated processing.
• Monitor Critical Muscle Biomarkers: Track Creatinine, SHBG, Albumin, and Cystatin C ratios to detect muscle catabolism weeks before DEXA scans reveal changes.
• Use AI-Powered Protein Targeting: Dynamically adjust protein intake above 1.2g/kg/day based on fat-free mass data to preserve muscle during weight loss.
• Plan Strategic Exit Protocols: Gradually taper GLP-1s over 9+ weeks while monitoring biological age with DunedinPACE to prevent metabolic crash and secure patient retention.
• Automate Workflow Systems: Reduce report preparation time by 56% (reclaiming 15 hours weekly) through automated protocol drafting and intelligent dashboards.
This muscle-centric approach transforms clinics from simple weight loss providers into strategic health architects, protecting patients from sarcopenia while maximizing the $200,000 lifetime value through comprehensive metabolic health management.
FAQs
Q1. What are the potential risks of GLP-1 therapies for weight loss? While GLP-1 therapies can be effective for weight loss, they may lead to significant muscle mass loss, potentially 15-40% of total weight lost. This can increase the risk of frailty and metabolic instability, undermining long-term health benefits.
Q2. How can clinics monitor muscle loss in patients using GLP-1 medications? Clinics can implement a ‘Muscle Defense’ dashboard that tracks key biomarkers such as Creatinine, SHBG, Albumin, and Cystatin C. Advanced neural networks can also detect subtle catabolism signals weeks before they appear on traditional scales or DEXA scans.
Q3. What strategies can help preserve muscle mass during GLP-1 therapy? Implementing an AI-powered nutrition platform that dynamically adjusts protein intake goals based on fat-free mass is crucial. Protein intake should be maintained above 1.2 g/kg/day, combined with structured resistance training to help preserve lean mass.
Q4. How should patients transition off GLP-1 medications safely? A safe transition involves gradual tapering over 9+ weeks or more, allowing patients to maintain or even continue losing weight. Close monitoring of protein turnover markers during this period is essential to prevent accelerated muscle catabolism.
Q5. What is DunedinPACE and why is it important in GLP-1 therapy management? DunedinPACE is a validated epigenetic biomarker that measures the pace of aging. It’s used as a “speedometer for aging” in GLP-1 therapy management, providing patients with visual evidence of their slowing biological aging. This can create powerful “Aha!” moments that drive long-term patient retention and engagement in their health journey.
References
[1] – https://pmc.ncbi.nlm.nih.gov/articles/PMC12564085/
[2] – https://www.trootech.com/blog/ehr-to-ai-clinical-intelligence-healthcare-it
[3] – https://www.bridgeheadsoftware.com/2025/02/overcoming-the-chaos-how-to-bring-order-to-your-clinical-data/
[4] – https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.066912
[5] – https://pmc.ncbi.nlm.nih.gov/articles/PMC3278860/
[6] – https://www.iqvia.com/solutions/technologies/orchestrated-clinical-trials/clinical-data-analytics-solutions/clinical-data-ingestion
[7] – https://pristacorp.com/insights/what-is-clinical-intelligence-benefits-importance/
[8] – https://pmc.ncbi.nlm.nih.gov/articles/PMC7950106/
[9] – https://diabetesjournals.org/care/article/48/7/1204/158057/Comparison-of-Serum-Creatinine-and-Cystatin-C
[10] – https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.1058464/full
[11] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8517349/
[12] – https://peterattiamd.com/ai-dexa-and-mortality/
[13] – https://www.sciencedirect.com/science/article/pii/S2405844023035302
[14] – https://pubmed.ncbi.nlm.nih.gov/29961893/
[15] – https://www.sciencedirect.com/science/article/abs/pii/S2405457722001620
[16] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9307489/
[17] – https://evidence.care/clinical-workflow-solutions/
[18] – https://pubmed.ncbi.nlm.nih.gov/35441470/
[19] – https://www.teladochealth.com/library/article/safely-stopping-glp-1-medication
[20] – https://moffittcaspi.trinity.duke.edu/dunedinpace
[21] – https://holisticare.io/blog/the-economics-of-patient-retention-for-longevity-clinics/
Disclaimer
The information in this article is provided by HolistiCare for general informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. HolistiCare does not warrant or guarantee the accuracy, completeness, or usefulness of any information contained in this article. Reliance on any information provided here is solely at your own risk.
This content does not create a doctor-patient relationship. Clinical decisions should be made by qualified healthcare professionals using clinical judgment and all available patient information. If you have a medical concern, contact your healthcare provider promptly.
HolistiCare may reference biomarker roles, study examples, products, or tools. Mention of specific tests, biomarkers, therapies, or vendors is for illustrative purposes only and does not imply endorsement. HolistiCare is not responsible for the content of third party sites linked from this article, and inclusion of links does not represent an endorsement of those sites.
Use of HolistiCare software, services, or outputs should be in accordance with applicable laws, regulations, and clinical standards. Where required by law or regulation, clinical use of biomarker information should rely on validated laboratory results and regulatory approvals. HolistiCare disclaims all liability for any loss or damage that may arise from reliance on the information contained in this article.
If you are a patient, please consult your healthcare provider for advice tailored to your clinical situation. If you are a clinician considering HolistiCare for clinical use, contact our team for product specifications, regulatory status, and clinical validation documentation.