AI in healthcare is rapidly transforming medical practice, with two-thirds of physicians already using health AI technologies. By 2030, the gap between supply of and demand for staff employed by NHS trusts could increase to almost 250,000 full-time equivalent posts, making technological solutions increasingly vital for healthcare delivery.
The potential of artificial intelligence in healthcare extends beyond addressing staffing shortages. Medical AI can analyze lab results and imaging faster and more accurately than humans, while healthcare AI applications facilitate efficient resource allocation through predictive modeling of patient admissions and optimization of hospital beds, staff, and equipment. Furthermore, there are currently more than 350,000 mobile health apps with AI frequently embedded in the software, and three out of 10 adults worldwide have used these applications, creating a market exceeding $70 billion annually.
Despite these advancements, you need to understand both the benefits and limitations of this technology. AI-driven personalized treatment plans can complement traditional approaches by offering more targeted care, but depending on how they’re trained, AI models can perpetuate biases and health disparities for certain populations.
This article explores essential AI tools for medical professionals, how artificial intelligence is changing clinical decision-making, the necessary training for an AI-enabled healthcare environment, regulatory considerations, and what the future holds for AI in medicine.
AI Tools Every Medical Professional Should Know in 2025
Medical professionals in 2025 now have access to an array of AI tools that enhance diagnostic accuracy, streamline workflows, and improve patient outcomes. Here are eight essential AI applications you should know about:
1. AI for Brain Scan Interpretation in Stroke Cases
AI software for stroke detection has dramatically improved patient outcomes, tripling recovery rates through faster diagnosis [1]. Tools like Brainomix 360 Stroke, deployed across England’s National Health Service, analyze brain scans for signs of tissue damage, reducing time to treatment from 140 to 79 minutes [2]. Moreover, this technology has increased the percentage of patients achieving functional independence from 16% to 48% [2]. Imperial College London researchers have also developed AI that can determine stroke onset time with twice the accuracy of visual assessment methods, potentially enabling 50% more patients to receive appropriate treatments [1].
2. Fracture Detection with AI in Emergency Rooms
AI-powered fracture detection systems demonstrate impressive accuracy in emergency settings. A study of pediatric radiographs showed 92% sensitivity and 83% specificity for fracture detection [3]. When pediatric residents used AI assistance, their diagnostic accuracy improved from 88% to 90% [3]. Similarly, another study of 1,500 radiograph sets from emergency department patients found AI effectively detected acute peripheral fractures [3]. In the UK, NICE has recommended four AI tools (TechCare Alert, BoneView, RBfracture, and Rayvolve) for fracture detection in urgent care settings [4].
3. Predictive Models for Ambulance Triage Decisions
A human-centered hybrid AI system for emergency triage combines cognitive modeling, machine learning, and resource optimization to provide interpretable recommendations [5]. This system achieved 90% accuracy and significantly reduced false negatives by 7% compared to baseline methods [5]. Additionally, it decreased clinician decision-making time by 31% and enhanced critical resource use by 20% [5]. In Thailand, an XGBoost model predicting ICU admissions achieved superior performance (AUROC 0.917) compared to traditional triage methods (0.882) [6].
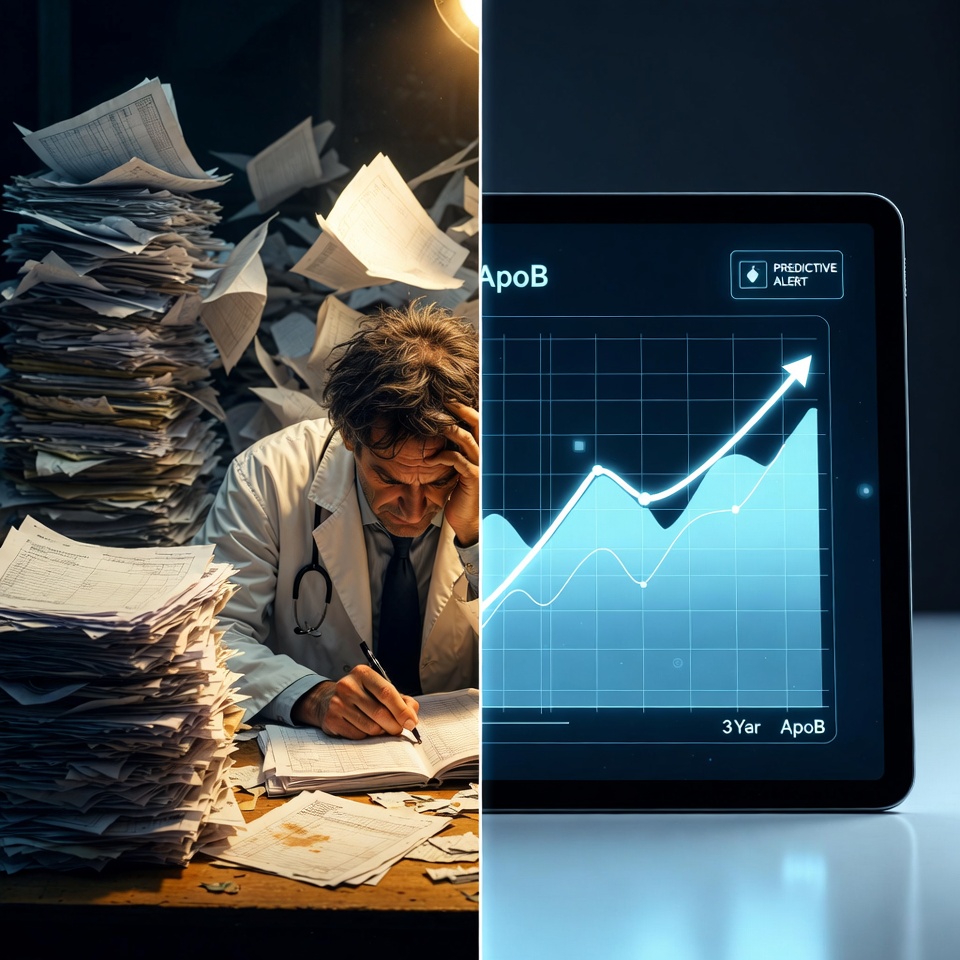
4. Early Disease Detection using Longitudinal Health Data
Longitudinal electronic health records contain valuable early indicators of disease that AI can identify. The Delphi-2M model predicts rates of over 1,000 diseases based on individual health histories [7]. This model provides disease burden estimates for up to 20 years and reveals clusters of co-morbidities and their time-dependent consequences [7]. A scoping review found that machine learning models can detect or predict conditions like diabetes, kidney diseases, and mental disorders earlier than current clinical diagnoses [8].
5. Clinical Chatbots for Patient Triage and Advice
AI chatbots now handle up to 80% of routine healthcare queries [9], providing 24/7 patient access to health information and symptom assessment [10]. These tools categorize patient conditions based on urgency—mild (self-care), moderate (primary care visit), or severe (emergency care) [9]—and integrate with electronic health records to ensure providers have complete patient information [9]. Although clinical evidence of chatbot effectiveness remains limited [10], they show promise in improving accessibility and reducing administrative burden.
6. AI Copilots for Clinical Documentation
Microsoft Dragon Copilot and similar tools capture patient-clinician conversations and automatically generate clinical notes [11]. Trained on over 15 million encounters, these systems produce accurate documentation efficiently [11]. At Novant Health, nearly 900 clinicians have used DAX Copilot in more than 550,000 patient encounters, reporting meaningful time savings per visit and improved work-life balance [12]. Furthermore, 87% of users believe these tools enhance the patient experience [12].
7. AI in Traditional Medicine and Ayurgenomics
The World Health Organization has recognized AI applications in traditional medicine systems [1]. Ayurgenomics—a fusion of Ayurvedic principles and genomics accelerated by AI—scans patient genomes against Ayurvedic parameters to propose personalized treatment regimens [2]. AI-powered diagnostic systems mimic traditional practices like pulse diagnosis and tongue examination [13], increasing diagnostic accuracy while minimizing practitioner variation [2]. Additionally, AI helps identify medicinal plants and analyze traditional medicine compounds for modern applications [1].
8. AI for Administrative Workflow Optimization
AI streamlines healthcare administration by automating routine tasks such as appointment scheduling, billing, and claims management [14]. These systems analyze historical data to predict staffing needs based on patient admissions and seasonal trends [15]. Consequently, AI reduces unnecessary overtime, better matches staff to patient demand, and limits reliance on costly agency staff [15]. AI-powered tools also generate optimized schedules that balance patient demand with nurse availability, reducing staffing costs by minimizing last-minute overtime [15].
How AI is Changing Clinical Decision-Making
“We need to design and build AI that helps healthcare professionals be better at what they do. The aim should be enabling humans to become better learners and decision-makers.” — Mihaela van der Schaar, PhD, Director of the Cambridge Center for AI in Medicine, University of Cambridge
AI-Supported Diagnosis vs Human Intuition
In diagnostic tasks, AI models sometimes demonstrate superior performance compared to human clinicians. For instance, the GPT-4 model had fewer errors in estimating pretest and posttest probabilities after negative results across five clinical cases [3]. This consistency stems from AI’s ability to process vast amounts of information without the cognitive biases that often affect human judgment.
Human diagnostic reasoning involves a complex interplay of cognitive, emotional, and intuitive factors [3]. Physicians rely on their five senses during patient interactions, gathering qualitative information that may be absent from electronic health records [4]. Conversely, AI operates systematically, providing a narrower distribution of responses across various scenarios [3].
Medical AI particularly excels at probabilistic reasoning. In one study, an AI model selected the correct diagnosis more often than physicians in closed-book settings, though physicians with access to reference materials outperformed AI, especially on the most challenging questions [16].
Certainly, AI has limitations. When describing medical images and explaining reasoning, AI models often make mistakes—even when arriving at the correct diagnosis [16]. In one example, an AI model failed to recognize that two differently angled lesions on a patient’s arm were caused by the same condition [16].
Combining AI Outputs with Clinical Judgment
Rather than simply accepting AI’s diagnostic output, expert clinicians are developing a new approach that begins with AI’s suggestion and works backward to assess its validity [5]. This verification process includes cross-referencing patient records and consulting with other experts [5].
Hence, the ideal future lies in human-AI symbiosis, where their respective abilities complement each other [4]. The “human-in-the-loop” model allows clinicians to guide how machines learn, providing intuition-based feedback [4]. This collaborative approach is particularly valuable as AI and human performance may vary across different patient populations [4].
Undoubtedly, healthcare organizations must hold AI developers accountable. Success should be measured not just in efficiency metrics but in clinical confidence, patient outcomes, and preservation of medical judgment [6]. As AI becomes more deeply embedded in clinical workflows, the responsibility remains with human clinicians to ensure these tools enhance rather than dilute the quality of care [17].
For medical professionals adapting to this new reality, the challenge isn’t whether AI will play a role in clinical reasoning—it already does. Instead, the question is whether it will be shaped in ways that deepen clinical judgment or diminish it [6].
Training and Upskilling for AI-Enabled Healthcare
Successful implementation of AI in healthcare depends fundamentally on a workforce equipped with the right skills. As frontline providers increasingly interact with AI systems, developing appropriate competencies has become a pressing necessity for medical institutions worldwide.
Digital Literacy for Medical Professionals
Digital health literacy among healthcare professionals extends beyond basic technology skills—it forms the cornerstone of effective patient care in today’s digitalized landscape [18]. This literacy exists in three distinct levels: functional (basic ability to obtain health information), interactive (extracting and applying information from various digital sources), and critical (analyzing information from multiple sources to make informed decisions) [19].
Many healthcare professionals currently lack adequate training to navigate the expanding digital environment, highlighting an urgent need for targeted education [18]. For nurses specifically, understanding AI fundamentals has become essential for ensuring safe and effective patient care [20]. Integrating digital health competencies into medical curricula prepares professionals to enhance patient engagement and address equity challenges in healthcare delivery [18].
AI Tool Onboarding and Simulation Training
AI-powered onboarding tools now streamline the traditionally complex process of introducing medical professionals to new technologies. These systems provide quick access to information, reduce overload, and help practitioners understand their roles more efficiently [7]. One notable benefit includes customized training pathways based on an individual’s existing knowledge level—for example, adjusting orientation processes based on a clinician’s understanding of cardiac rhythm or diabetic care [7].
Simulation training with AI has proven particularly valuable. Studies show AI-based simulators create highly realistic clinical scenarios, allowing medical students to practice repeatedly with consistent experiences at reasonable costs [21]. Virtual patients powered by natural language processing enable realistic doctor-patient conversations, providing safe environments for developing communication skills [8]. These simulation technologies automatically analyze learners’ actions and decisions, creating personalized feedback and adapting scenarios to individual learning needs [22].
Several major universities now offer comprehensive AI training programs covering essential concepts, practical applications, and ethical considerations—addressing the shortage of instructors with expertise in clinical AI applications [23].
Regulatory and Safety Considerations for AI Tools
Regulatory frameworks for AI in healthcare are presently evolving to address safety and ethical considerations unique to this rapidly advancing field.
FDA and EU AI Act Compliance Requirements
The EU AI Act, which entered into force in August 2024, establishes a risk-based framework that classifies AI systems into distinct categories [24]. Medical device AI systems qualify as “high-risk” under the Act if they function as safety components or are medical devices themselves [25]. This classification triggers comprehensive compliance requirements including rigorous risk management, data governance, and technical documentation [10].
The Act has an extra-territorial reach, applying to any AI provider placing systems on the EU market or whose output is used in the EU, regardless of location [10]. Implementation follows a phased approach: prohibited AI provisions apply from February 2025, while most high-risk AI requirements become applicable in August 2026 [24].
Evaluating AI Tool Accuracy and Hallucination Risks
AI hallucinations—the generation of content not based on real data but produced through creative interpretation of training data—pose significant risks in healthcare [26]. In one study, an AI system fabricated fictional medications like “hyperactivated antibiotics” [9], highlighting potential patient safety concerns.
According to a national analysis of 2,425 U.S. hospitals, approximately 65% use AI-assisted predictive models [27]. However, only 61% evaluated these models for accuracy and just 44% for bias [27]. This evaluation gap creates a digital divide between resource-rich institutions that can develop and test their own models versus under-resourced hospitals using off-the-shelf solutions [27].
Data Governance and Patient Consent Models
Effective health data governance is essential for creating trusted AI systems that deliver high-quality, equitable care [28]. For high-risk AI tools, the EU AI Act requires robust data governance that aligns with GDPR while adding AI-specific requirements related to training, validation, and testing datasets [10].
Patient consent considerations vary based on AI implementation. A recent study found that 77% of patients reported being comfortable with their physician using ambient documentation technology, yet 59.2% did not want their data shared with the technology vendor [29], illustrating the need for transparent consent models.
Future Outlook: What’s Next for AI in Medicine?
Beyond current applications, the next frontier of AI in medicine promises even more profound advancements that will reshape healthcare delivery systems worldwide.
Digital Twins for Personalized Treatment Simulation
Digital twin technology creates virtual replicas of individual patients, enabling physicians to test treatments before actual implementation. These computational models simulate how specific patients might respond to various interventions based on their unique biological characteristics. Currently, researchers are developing digital twins that incorporate multi-omics data alongside traditional health records, creating unprecedented opportunities for precision medicine.
Ambient Intelligence in Smart Hospitals
Smart hospitals equipped with ambient intelligence are emerging as the future standard of care facilities. These environments continuously monitor patients through unobtrusive sensors embedded throughout clinical spaces. Eventually, AI systems will autonomously adjust room conditions, anticipate patient needs, and alert staff to potential issues before they become critical—effectively creating responsive healing environments that adapt in real-time to patient conditions.
AI-Driven Drug Discovery and Genomics Integration
The integration of AI with genomics is revolutionizing drug discovery processes. Indeed, AI algorithms now screen billions of potential molecular compounds, drastically reducing development timelines from years to months. In fact, multiple AI-discovered drug candidates have already entered clinical trials. Soon, physicians will prescribe treatments based on a patient’s complete genetic profile, with AI systems identifying optimal drug combinations that account for individual genetic variations and potential adverse reactions.
Conclusion
Artificial intelligence stands at the forefront of healthcare transformation, fundamentally reshaping how you practice medicine. Throughout this article, you have seen how AI tools enhance diagnostic accuracy, streamline administrative tasks, and improve patient outcomes across numerous clinical scenarios. These technologies offer powerful solutions to address growing staffing shortages while simultaneously increasing the precision and efficiency of medical care.
Despite their impressive capabilities, AI systems cannot replace your clinical judgment. Instead, they function best as augmentative tools that complement your expertise. The most effective approach combines AI’s computational power with your human intuition, creating a symbiotic relationship that elevates patient care beyond what either could achieve alone.
Preparing for this AI-enabled future requires deliberate upskilling. Digital literacy, proper tool onboarding, and simulation training have become essential components of medical education. Additionally, understanding the evolving regulatory landscape helps you navigate compliance requirements while maintaining ethical standards in AI implementation.
Looking ahead, digital twins, ambient intelligence, and AI-driven drug discovery promise even greater advancements. These technologies will undoubtedly transform healthcare delivery, though their successful integration depends on thoughtful implementation that preserves the human elements of medicine.
The AI revolution in healthcare has already begun. Your ability to adapt, critically evaluate these tools, and integrate them judiciously into clinical practice will determine how effectively they serve patients. The goal remains unchanged—providing optimal care—but the methods continue to evolve, offering unprecedented opportunities to enhance your clinical capabilities while addressing healthcare’s most pressing challenges.
Key Takeaways
AI is revolutionizing healthcare delivery, with medical professionals needing to understand both the transformative potential and practical implementation of these technologies in 2025.
• AI tools dramatically improve diagnostic speed and accuracy – Brain scan interpretation for strokes tripled recovery rates, while fracture detection systems achieve 92% sensitivity in emergency settings.
• Human-AI collaboration enhances clinical decision-making – The most effective approach combines AI’s computational power with physician intuition, requiring verification of AI outputs through clinical judgment.
• Digital literacy and targeted training are essential – Medical professionals need comprehensive upskilling in AI fundamentals, simulation training, and tool onboarding to safely integrate these technologies into practice.
• Regulatory compliance and safety evaluation are critical – The EU AI Act classifies medical AI as “high-risk,” requiring rigorous testing for accuracy and bias, while only 44% of hospitals currently evaluate AI tools for bias.
• Future innovations will personalize medicine further – Digital twins, ambient intelligence, and AI-driven drug discovery will enable unprecedented precision in treatment while maintaining the irreplaceable value of human clinical expertise.
The successful integration of AI in healthcare depends on medical professionals who can critically evaluate these tools while preserving the human elements that define quality patient care.
FAQs
Q1. How is AI improving diagnostic accuracy in healthcare? AI tools are significantly enhancing diagnostic accuracy in various medical fields. For example, AI software for stroke detection has tripled recovery rates by reducing time to treatment from 140 to 79 minutes. In fracture detection, AI systems have demonstrated 92% sensitivity in emergency settings, improving diagnostic accuracy of pediatric residents from 88% to 90% when used as an assistive tool.
Q2. What role does AI play in clinical decision-making? AI is becoming an integral part of clinical decision-making, often demonstrating superior performance in diagnostic tasks compared to human clinicians. However, the ideal approach is a human-AI symbiosis, where AI’s computational power complements the clinician’s expertise and intuition. This collaborative model allows for more accurate diagnoses and treatment plans while preserving the critical role of human judgment in patient care.
Q3. How are medical professionals being trained to use AI in healthcare? Medical professionals are being trained through various methods to effectively use AI in healthcare. This includes developing digital health literacy at functional, interactive, and critical levels. AI-powered onboarding tools provide customized training pathways, while simulation training with AI creates realistic clinical scenarios for practice. Many universities now offer comprehensive AI training programs covering essential concepts, practical applications, and ethical considerations.
Q4. What are the regulatory considerations for AI in healthcare? Regulatory frameworks for AI in healthcare are evolving rapidly. The EU AI Act, which came into force in August 2024, classifies medical device AI systems as “high-risk,” triggering comprehensive compliance requirements. These include rigorous risk management, data governance, and technical documentation. Additionally, there’s an increasing focus on evaluating AI tools for accuracy and bias, as well as establishing robust data governance and patient consent models.
Q5. What future developments can we expect in AI-driven healthcare? The future of AI in healthcare promises even more advanced applications. Digital twins technology will enable personalized treatment simulations based on individual patient characteristics. Smart hospitals equipped with ambient intelligence will continuously monitor patients and autonomously adjust care environments. AI-driven drug discovery integrated with genomics is expected to revolutionize treatment development, potentially reducing drug development timelines from years to months.
References
[1] – https://www.who.int/news/item/11-07-2025-who–itu–wipo-showcase-a-new-report-on-ai-use-in-traditional-medicine
[2] – https://m.economictimes.com/ai/ai-insights/india-takes-a-lead-in-the-world-by-digitizing-traditional-medicine-using-an-ai-based-library-/articleshow/122833583.cms
[3] – https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2812737
[4] – https://pmc.ncbi.nlm.nih.gov/articles/PMC7481865/
[5] – https://www.nature.com/articles/s41746-025-01460-1
[6] – https://www.medicaleconomics.com/view/don-t-dilute-the-art-of-medicine-how-ai-can-support-clinical-judgment
[7] – https://c8health.com/a/blog/optimizing-onboarding-workflow-with-ai-powered-tools-and-alerts
[8] – https://oxfordmedicalsimulation.com/artificial-intelligence-in-healthcare-simulation-the-why-and-how/
[9] – https://www.cio.com/article/3593403/patients-may-suffer-from-hallucinations-of-ai-medical-transcription-tools.html
[10] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11379845/
[11] – https://www.microsoft.com/en-us/health-solutions/clinical-workflow/dragon-copilot
[12] – https://supportnovanthealth.org/ai-technology-is-reinventing-clinical-documentation-increasing-team-member-well-being/
[13] – https://www.newsonair.gov.in/who-recognizes-indias-pioneering-efforts-in-integrating-ai-with-traditional-medicine-particularly-ayush-systems/
[14] – https://www.keragon.com/blog/ai-in-healthcare-administration
[15] – https://www.shiftmed.com/insights/knowledge-center/impact-of-ai-in-healthcare-administration/
[16] – https://www.nih.gov/news-events/news-releases/nih-findings-shed-light-risks-benefits-integrating-ai-into-medical-decision-making
[17] – https://www.nature.com/articles/s41746-025-01725-9
[18] – https://pmc.ncbi.nlm.nih.gov/articles/PMC12176768/
[19] – https://www.tandfonline.com/doi/full/10.1080/28355245.2023.2263355
[20] – https://www.sciencedirect.com/science/article/pii/S0029655425001198
[21] – https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-024-06236-x
[22] – https://www.nursingsimulation.org/article/S1876-1399(23)00070-1/fulltext
[23] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11822726/
[24] – https://www.hunton.com/insights/legal/the-impact-of-the-eu-ai-act-on-the-development-and-use-of-medical-devices
[25] – https://viewpoints.reedsmith.com/post/102kq35/the-eu-ai-act-and-medical-devices-navigating-high-risk-compliance
[26] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10552880/
[27] – https://www.sph.umn.edu/news/new-study-analyzes-hospitals-use-of-ai-assisted-predictive-tools-for-accuracy-and-biases/
[28] – https://www.who.int/europe/publications/i/item/WHO-EURO-2025-11462-51234-78079
[29] – https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2836694